19100006004 CASE PRESENTATION
LONG CASE :
CHEIF COMPLAINTS :
29/F came to OPD with C/o Loss of appetite , weight since 2 years
Generalised weakness and easy fatiguability since 2 years .
C/o Fever since 6 months
C/o Multiple joint pains and swelling since 6 months
Difficulty in movements and walking since 6 months.
C/o Hyper-pigmented leisons over cheeck bones and chin ,ears , b/l fore arm since 4 months .
C/o Severe hair loss since 4 months .
HOPI AND PAST HISTORY :
NO H/o chest pain, shortness of breath ,PND.
NO H/o bluish ,white discoloration of limbs on exposure to cold .
No h/o dry eyes and dry mouth .
FAMILY HISTORY :
No family history of joint pains/ other auto-immune diseases.
Younger sister SCD .
EDUCATIONAL STATUS :
Patient completed her BA .
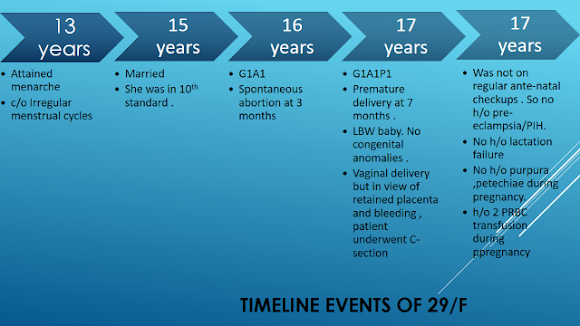
MARITAL HISTORY :
Married at 15 years of age . But divorced at 20 years of age.
SOCIAL HISTORY :
Poor socio-economic status .
PROVISIONAL DIAGNOSIS :
PROBLEM REPRESENTATION :
- H/o recurrent abortions , and young onset CVA , Seizures suggests ? HYPER-COAGULABLE STATE
-29/F with recurrent history of fever and multiple joint pains , rash and hair loss , loss of appetite and weight ,fatigue - all point towards auto immune etiology ,especially in a young female .
2-3 year history of bilaterally symmetrical ,chronic progressive inflammatory polyarthritis predominantly involving small joints .
Features favouring an inflammatory pathology are -
- Features of inflammation such as severe pain associated with edema of the joints and limitation of range of active movements
- Early morning stiffness, lasting for more than 30 mins (for 1 hour in this patient)
- Pain and edema of joints improving with activity and worsening with rest
- Features of uncontrolled systemic inflammation such as fever, involuntary loss of weight associated with loss of appetite.
- Swellings at joints and deformation of normal joint posture
Provisional Diagnosis - Bilaterally Symmetric Chronic Progressive Inflammatory Peripheral Polyarthritis
GENERAL EXAMINATION :
Head to Toe General Examination
Systemic Examination
Musculo-Skeletal System :
JOINTS | RIGHT | LEFT |
1)SHOULDER JOINT a) Inspection : Attitude of limbs –
Swelling – Skin - Deformity – Muscle wasting –
b)Palpation :
Tenderness – Warmth – Synovial thickening – Crepitus –
c) Range of movements : Active Passive
|
Slightly flexed and internally rotated; Contour normal NO NO ERYTHEMA NO NO
All inspiratory findings confirmed YES NO NO NO
Slight limitation of active and passive extension and overhead abduction |
Slightly flexed and internally rotated; Contour normal NO NO ERYTHEMA NO NO
All inspiratory findings confirmed YES NO NO NO
Slight limitation of active and passive extension and overhead abduction |
2)ELBOW JOINT a) Inspection : Attitude of limbs –
Swelling – Skin - Deformity – Muscle wasting –
b)Palpation : Tenderness – Warmth – Synovial thickening – Crepitus –
c) Range of movements : Active Passive
|
Attitude - mid-flexion; alignment of elbow and forearm - normal; YES NO erythema No No
YES SLIGHT NO NO
No restriction | Attitude - mid-flexion; alignment of elbow and forearm - normal; NO NO erythema No No YES NO NO NO
No restriction |
3)WRIST JOINT: a) Inspection : Attitude of limbs – Swelling – Skin - Deformity – Muscle wasting –
b)Palpation : Tenderness – Warmth – Synovial thickening – Crepitus –
c) Range of movements : Active Passive
|
MILD EXTENSION
No No No No
Yes No No No
Limitation of active and passive ulnar deviation |
MILD EXTENSION
No No No No
Yes No No No
Limitation of active and passive ulnar deviation |
4)HANDS (small joints) a) Inspection : Attitude of limbs – Swelling – Skin - Deformity – Muscle wasting –
b)Palpation : Tenderness – Warmth – Synovial thickening – Crepitus –
c) Range of movements : Active Passive
|
Fingers flexed at MCP and PIP MILD NO ERYTHEMA NO NO
Present at MCP,PIP NO NO NO
Slight Limitation of passive flexion at MCP |
Fingers flexed at MCP and PIP MILD NO ERYTHEMA NO NO
Present at MCP,PIP NO NO NO
Slight Limitation of passive flexion at MCP |
5)HIP JOINT : a) Inspection : Attitude of limbs – Swelling – Skin - Deformity – Muscle wasting –
b)Palpation : Tenderness – Warmth – Synovial thickening – Crepitus –
c) Range of movements : Active Passive
|
Slight flexed and internal rotated NO NO erythema No No
Yes No No No
Limitation of passive and active movements of flexion and extension. (towards the end of range of motion); |
Slight flexed and internal rotated NO NO erythema No No
Yes No No No
Limitation of passive and active movements of flexion and extension( towards the end of range of motion); |
6) KNEE JOINT : a) Inspection : Attitude of limbs – Swelling – Skin - Deformity – Muscle wasting –
b)Palpation : Tenderness – Warmth – Synovial thickening – Crepitus –
c) Range of movements : Active Passive
|
MILD NO erythema No No
Yes No No No
No restriction |
MILD NO erythema No No
Yes No No No
No restriction |
7) ANKLE JOINT: a) Inspection : Attitude of limbs – Swelling – Skin - Deformity – Muscle wasting –
b)Palpation : Tenderness – Warmth – Synovial thickening – Crepitus –
c) Range of movements : Active Passive
|
Dorsiflexed Yes (minimal) No No No
Yes Slight No No
Limitation of passive and active plantar flexion |
Dorsiflexed Yes No No No
Yes Slight No No
Limitation of passive and active plantar flexion |
8) FEET EXAMINATION : a) Inspection : Attitude of limbs –
Swelling – Skin - Deformity – Muscle wasting –
b)Palpation : Tenderness – Warmth – Synovial thickening – Crepitus –
c) Range of movements : Active Passive
|
Foot hanging on side of bed
No No No No
Yes at MTP,PIP NO No No
Limitation of passive movements of flexion and extension of MTP joints
|
Foot hanging on side of bed
No No No No
Yes at MTP ,PIP NO No No Limitation of passive movements of flexion and extension of MTP joints
|
|
|
|
|
|
|
Is associated with a worse prognosis and higher mortality from the disease.12,16,17 It has been linked with a severe disease course including neuropsychiatric disorders, renal involvement, hemolytic anemia and antiphospholipid syndrome.The leading cause of death in the Reveille et al.20 study was infection.In two large studies thrombocytopenia was the only independent predictor for mortality in SLE.
19 year old male resident of Nalgonda and currently studying intermediate ,came to opd with complaints of :
-Itchy Ring leisons over arms ,abdomen ,thigh and groin since 1 and half year .
-Purple stretch marks all over abdomen ,lower back ,upper limbs ,thighs since 1 year .
-Abdominal distension and facial puffiness since 6 months.
- Pedal edema since 3 months.
- Low back ache since 3 months .
- Feeling low , not feeling to talk to anyone.
- Weight gain and decreased libido since 3months.
- Loss of libido and erectile dysfunction since 2 months .
Pt was apparently alright one and half year ago , when he slowly developed erythematous round leisons which are annular shaped and itchy all over abdomen , upper limb ,groin and inner thigh region .
No history of fever back then. No other complaints apart from skin lesions.
Pt visited local RMP where he prescribed auyurvedic medications and other creams ( unknown composition as pt don't have them currently ). He also prescribed tablets (unknown composition) . Patient started using all these medications for 1-2 months .
Leisons reduced a bit after using medications .
Later after 2 months he developed multiple hyper pigmented plaques over lower limbs ,abdomen , for which he again visited same place and used ayurvedic oils over the leisons.
He also used clobetasol ointment over the leisons.(for approximately 1 year all over the body)
He started noticing pink striae over his abdomen first 1 year ago and later on back and over arms,which were gradually increasing in size .
Later he visited a hospital and used miconazole and luliconazole ointments also.
He used clobetasol ointment all over the leisons for long time .
He started noticing abdominal distension and facial puffiness ,weight gain, but never visited any hospital.
Later he developed pedal edema and low back ache since 3 months .
His consulted a dermatologist at this point of time who advised to consult physician and prescribed monteleukast , itraconazole tablets ,luliconazole ointment for tenia corporis.
He stopped all medications one month ago and visited our opd with complaints of pink striae and easy fatigue ,weakness and low back ache .
His brother also gave history of pt being moody and feeling of low self esteem due to multiple leisons.
He even complaints pt wouldn't step out of house and always stays indoor and wouldn't interact with others .
No complaints of chest pain ,sob , palpitations .
No complaints of decreased or frothy urine.
No other negative history.
No h/o DM,HTN,TB,ASTHMA,CAD.
ALLERGIC HISTORY - pt gives h/o allergy to eggs ,brinjal .
O/E : Pt was c/c/c
BP - 160/100 mmHg
Pr - 96 BPM ,regular ,normovolemic .
Rr - 18/min
Spo2- 98% on ra.
Weight - 63 kg.
Height - 175 cm.
GENERAL EXAMINATION :
NO pallor ,icterus ,cyanosis , clubbing, lymphadenopathy.
Pedal edema present - pitting type extending upto knee.
Abdominal distension present.
Moon face present
Pink striae noted over anterior abdominal wall and on low back and on upper arms and thighs.
Thin skin present .
Poor healing noticed over leg ulcers and easy bruising noted .
Acne present over face .
Acanthosis nigrans noted over neck.
GYNECOMASTIA PRESENT .
neck pad of fat present .
Sparse scalp hair .
.
Skin examination - Multiple itchy erythematous annular leisons noted all over abdomen , upper limb ,groin and inner thigh region .
Multiple hyperpigmented plaques noted over bilateral lower limbs .
SYSTEMIC EXAMINATION :
CVS - S1S2 heard .No murmurs
RS - BAE present .
No adventitious sounds .
P/A - Soft , distended .
No organomegaly .
Bowel sounds present .
CNS - HMF - INTACT R. L
MOTOR SYSTEM - POWER - UL 5/5 5/5
LL 5/5 5/5
Proximal muscles lower limb - power is 4/5 .
TONE - NORMAL.
REFLEXES - B. T. S. K. A. P
R. +2 +2. +1. +2. +1. FELXOR
L. +2. +2. +2. +2. +1. FLEXOR.
CRANIAL NERVES - NORMAL .
Difficulty in getting up from chair was noticed.
PROVISIONAL DIAGNOSIS -
? IATROGENIC CUSHINGS SYNDROME .
TINEA CORPORIS .
DENOVO HTN .
INVESTIGATIONS :
CBP - HB - 13.4 g/dl
TLC - 6,800
PLT - 1.5 lakhs.
RBS - 139 mg/dl
CUE - ALBUMIN - +1
SUGARS - NIL .
PUS CELLS - 3-4
RBC - NIL .
LFT - TB -1.03
DB-0.21
ALBUMIN - 3.9
RFT - UREA - 22
SERUM CREATININE -0.6
ELECTROLYTES - NA - 136
K- 4
CL-98
USG ABDOMEN - NORMAL.
ECG - SINUS TACHYCARDIA
LVH PRESENT.
This was picture of striae one year ago when it gradually started :
On presentation to opd pictures : 28/05/21
We took dermatologist opinion for tenia corporis where they advised
Ointment AMLORFINE
FUSIDIC ACID CREAM.
SALINE COMPRESS OVER LEISONS.
Plan to start anti fungals on next visit once dose of steroids is reduced .
OPTHAL opinion Was taken to look for visual acuity and cataract .
No features of lens opacities noted .
BUT IOP was high ,where they advised to follow up .
We advised pt to get fasting 8am serum cortisol levels and was planned to start on low dose steroids to avoid adrenal crisis.
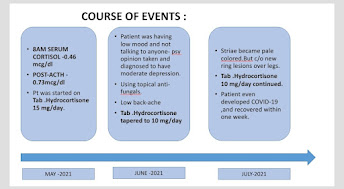
8AM S CORTISOL LEVELS (30/5/21)
- 0.46 mcg/dl ( very low) .
( normal range - 4.3-22.4 mcg/dl).
In view of lvh pt was started on tab telma 20 mg od .
On 3/6/21 - ACTH STIMULATION TEST WAS DONE .
BY INJECTING 0.4 ML OF ACTOM PROLONGATUM INJECTION (ACTH) INTRA MUSCULAR @ 7am
1 HR LATER FASTING SERUM CORTISOL SAMPLE WAS SENT .
VALUE - 0.73 mcg/dl
Indicating there was HPA AXIS suppression and pt was started on TAB HIZONE 15 mg per day in three divided doses @ 8am ,12 pm and 4 pm.
Pt was asked to follow up after one month .
FINAL DIAGNOSIS :
IATROGENIC CUSHINGS SYNDROME SECONDARY TO TOPICAL CLOBETASOL APPLICATION ALL OVER BODY FOR APPROXIMATELY ONE YEAR.
TINEA CORPORIS
DENOVO HTN .
FOLLOW UP -
ON NEXT VISIT : ( 25/6/21).
Pt was symptomatically better , pedal edema subsided.
Striae were pale in color and we're subsiding.
Weight - 67kg
Ht -175 cm.
Bp- 160/100 mmHg.
Pr -88bpm.
Dose of Tab hizone was reduced to 10 mg per day in divided doses for one month.
In view of low back ache Xray LS spine was done which was normal and pt was advised.:
Tab Shelcal 500 OD and Tab Vit D 3 Od.
Tab ULTRACET /PO/SOS.
Psychiatry opinion was taken and he was diagnosed with moderate depression .
In July 2021 pt was complaining of fever ,sore throat and dry cough since 3 days and he was tested positive for COVID 19 , we advised him home isolation and PCM 650 Mg /po /tid x 5 days .
He was advised to continue tab hizone tablets as it was advised. ( 10mg/day in divided doses.)
-INJ HYDROCORTISONE 100mg sos if pt is in adrenal shock.
He recovered from COVID within one week .
Next visit : ( 6/8/21).
BP- 170/100 - TELMA DOSE WAS INCREASED TO 40 MG OD.
PR - 88bpm.regular , normovolemic.
Wt- 69 kg
Height -
Abdominal girth - 96cm
Pt complaints of excoriation over striae and appearance of erythematous macules over abdomen whenever he takes food he is allergic to.
Took dermatologist opinion for it . They started him on Tab Itraconazole 100 mg bd for 2 weeks. And lulifin cream and tab levocitrixine 5mg od.
His brother complaints of depressed mood , pt not going out due to social stigma. Psychiatric counselling was given .
He still complaints of low back ache..othropedics opinion was taken and advised to continue Ultracet and tab Shelcal .
Cbp , cue and electoltes were repeated which were all in normal range .
USG ABDOMEN was done - Normal kidney size bilateral and CMD maintained. No other sonological abnormality noted.
As his lesions dint subside we reduced dose of hisone to 7.5 mg per day ,to see response.
Review psychiatry and opthal opinion was taken , where his lens was clear - no e/o cataract .
no retinopathy changes and no raised IOP and his visual acuity was 6/6.
0N 20/8/21 - IN view of constant low back ache , MRI LS SPINE WAS done with whole soine screening .
which showed lumbar epidural lipomatosis .
Mild depression of superior endplates of D12 and L4 - Likely subacute /chronic compression .
L3-L4 disc degeneration with mild diffuse disc bulge causing no significant neural foramen stenosis .
ON 24/8/21 - Pt developed painful swelling and redness of right lower limb along with intermittent fever - DIAGNOSED TO HAVE RIGHT LOWE LIMB CELLULITIS .
Pt was admitted and was given IV AUGMENTIN for 5 days and MGSO4 dressings were done .
TAB chymerol forte was given for 5 days.
Tab hisone 7.5 mg was continued in divided doses .
-INJ HYDROCORTISONE 100mg sos if pt is in adrenal shock.
PT again came for follow up in september , complaints of weight gain , but striae reduced and patient attender was giving history of patient having low mood and constantly being at home and not doing any exercise .
He was having social inhibition and was avoiding contact with other people.
We sent him for psychiatry where brief counselling was given .
TAB HISONE dose was reduced to 5 mg /day.
Next follow up was in october (22/10/11) ,pt improved and dose was further reduced to 2.5 mg/day .
PT again visited to our OPD on 23/ 11/21 , again with
c/o increasing striae and abdominal distension.since one month .( Striae were same as before ,but pt was feeling that way )
Abdominal distension could be due to fat accumulation,as pt was hardly exercising and is only staying at home and eating food.
weight gain present .( 76kg ).
c/o diminished vision
BP-160/100 mmhg
PR - 110 bpm
CVS- S1 S2 PRESENT
RS - BAE present and clear .
Pt was giving history of good compliance to medications and was using tab hisone 2.5mg only since past one month .No history of other medications ( ayurvedic or homeopathic ) usuage .
He is still having social inhibiton and is not going out of house or doing regular exercise .
P is having lot of anxiety and psychiatric issues.
As his blood pressure is uncontrolled and ECG having LVH - we increased the dose of anti-htn to TAB TELMA AM 40/5 mg OD.
HIS ROUTINE investigations were repeated , cbp,s. electrolytes ,s.creat was normal .
HIS RBS was 178 mg/dl
HBA1C was 6.5 %
Review Dermat opinion was taken ,
PT dint use his cream and itraconazole tablets regularly last month .
Review psychiatry opinion taken - Adjustment issues due to underlying illness.
Brief psychotherapy given .
REVIEW ENDOCRINE OPINION TAKEN (26/11/21) : Pt apprehensive .
Stopped hisone 2.5 mg and observe patient.
Only stress dose - Inj hydrocortisone 100 mg IV IF PT IS IN Adrenal shock .
Adv -8am serum cortsiol
65 year old male patient r/o Nakrekal presented to casualty with complaints of
C/O Shortness of breath grade 3 since 4 months .
C/O B/L pedal edema since 4 months .
C/O abdominal distension since 5 days
C/O Oliguria since 2 days
HISTORY OF PRESENTING ILLNESS :
Patient is toddy climber by occupation , was apparently asymptomatic 4 months ago .
-Intially he noticed b/l swelling of lower limbs , gradual onset and progressive . Pitting type and extending upto knees .
Associated with shortness of breath grade 2 , progressed to grade 3 over 4 months .
H/O orthopnea and PND present .
No h/o chest pain , palpitations
In view of sob , patient visited local hospital and was told ,he had a stone in one of his kidneys and both his kidneys failed .
He was advised maintainace hemodialysis,but patient denied and was discharged on medications .
His pedal edema subsided after using medications .
He continued taking medications , but noticed loss of appetite, weight , fatigue and generalized weakness .
His urine output was adequate previously . H/o hematuria present occasionally
No h/o pus in urine , burning micturition , frothy urine .
As he had generalized fatigue ,loss of appetite and ,sob ,elevated urea and s. creatinine he visited our hospital and was initiated on hemodialysis by placing central venous catheter in right internal jugular vein .
Patient had 4 sessions of hemodialysis .
He went to Hyderabad and got A-V fistula on his left hand .
C/o Low back ache and body pains .
C/O abdominal distension since 5 days , sudden onset and progressed gradually . Associated with increased sob on lying down and abdominal tightness.
Pedal edema is mild extending upto ankle joint.
No h/o yellowish discoloration of eyes . No h/o binge alcohol intake .
Past history - K/c/o HTN since 10 years and is not on regular medication .
NOT a k/c/o DM, TB , ASTHMA,CAD , EPILEPSY,CVA .
No surgical history and past Medical history
No h/ o NSAID abuse .
Personal history - Regular bowel and bladder movements
Adequate sleep
Loss of appetite present
Mixed diet
Social & Educational History :
Married for 27 years with 2 children. Not educated
Family history - Not significant
Addictions - Toddy drinker occasionally -3 times /week . 90 ml
Non -Smoker
PROVISIONAL DIAGNOSIS :
65 year old male with acute history of oliguria and abdominal distension ,on a background of Sob and pedal edema and HTN
?Acute decompensated Heart failure in view of anasarca and orthopnea and PND .
? Renal failure in view of decreased urine output and Anasarca and h/o renal calculi and HTN
General examination :
Pt C/C/C
Pallor - present
No icterus , clubbing, cyanosis,koilonychia , lymphadenopathy
B/L pedal edema - pitting type present. extending upto ankle .
Jvp - couldn't be assessed due to central line .
Skin - Dry ,scaly , itching present .
Eyes - Grade 2 HTN retinopathy changes noted on fundoscopy .
Vitals :
Bp - 140/90 mmhg - Right arm supine posture
Pulse - 130 bpm ,regular ,normal volume, condition of vessel wall - normal, no radio-radial or radio-femoral delay.
Resp rate - 26/ min
Spo2 - 97% on RA
Grbs - 110 mg/dl
Temp -99 F
SYSTEMIC EXAMINATION :
GIT EXAMINATION :
INSPECTION :
Shape of abdomen - Distended-uniform
Flanks – Full
Umbilicus – Everted
Skin – Stretched, shiny
No scars, sinuses, striae, nodules , discoloration.
Dilated veins – on front present
Movements of the abdominal wall - All quadrants equally moving with respiration .
Abdomino - Thoracic type of breathing
NO visible intestinal peristalsis
Hernial Orifices normal
Cough impulse - Negative
External genitalia - Scrotal swelling present
PALPATION :
Measurements - Abdominal Girth - 108 cm
Flanks - full
Superficial Palpation – Tenderness present in epigastrium
No local rise of temperature
Direction of Blood Flow in Veins - away from umbilicus
Deep Palpation :
Liver Span - Couldn't be palpalted due to gross distension .
Spleen - Couldn't be palpalted due to gross distension
Kidney - Couldn't be palpalted due to gross distension
Any other Palpable swelling - No
Hernial Orifices - normal
Murphy’s Punch/Renal angle tenderness - no tenderness
External Genitalia - scrotal edema present . non tender and trans -luminant
PERCUSSION:
Fluid Thrill - Present
Shifting dullness - Present
AUSCULTATION:
Bowel sounds – Present
Aortic, Renal Bruit - Absent
CARDIOVASCULAR EXAMINATION :
INSPECTION:
Chest wall shape - Ellipsoid and b/l symmetrical
No Precordial bulge, Pectus carinatum/excavatum
No Kyphoscoliosis
No Dilated veins, scars, sinuses
Apical impulse - Visible in left 5 ICS 1 cm lateral to MCL .
Pulsations – epigastric, parasternal - absent
PALPATION:
Apical impulse – Tapping type , felt in left 5 ICS 1 cm lateral to MCL .
Pulsations – No Epigastric pulsations
Parasternal Heave – Present - Grade 2
No Thrills and palpable heart sounds .
Auscultation :
S1 S2 heard in Aortic , pulmonary,tricuspid and mitral areas .
No added sounds
No murmurs
Respiratory system -B/L NVBS
B/L fine crepitations present IAA ,ISA .
CNS - NO abnormality detected .
INVESTIGATIONS :
BGT:- A positive
Serum iron :- 83
CBP :
HB - 7 g/dl
TLC - 12,400 cells /mm3
Platelets -1.3 lakhs .
RFT:-
Urea :- 92 mg/dl
Creatinine :- 5.7 mg/dl
Uric acid :- 6.6 mg/dl
Calcium :- 9.6 mg/dl
Phosphorus :- 3.4 mg/dl
Sodium :- 132 mEq /L
Potassium :- 3.7 mEq/L
Chloride :- 98 mEq/L
RBS:- 79mg/dl
LFT:-
Total bilirubin :- 2.12 mg/dl
Direct bilirubin:- 0.64 mg/dl
AST :- 17 IU/L
ALT :- 10 IU/L
Alkaline phosphatase:- 203 IU/L
Total proteins :-6.1 gm/dl
Albumin:- 2.2 gm/dl
A/G ratio:- 0.56
USG SCANNING OF WHOLE ABDOMEN:-
Impression:-
1) Bilateral GRADE 3 RENAL PARENCHYMAL CHANGES
2) MULTIPLE LARGE LEFT RENAL CALCULI .
3) Moderate to Gross ascitis
COMPLETE URINE EXAMINATION:-
Colour:- pale yellow
Appearance :- slightly hazy
Specific gravity:- 1.010
PH:- Acidic (6.0)
Proteins:- +++
Glucose :- Nil
Urobilinogen:- Negative
Bilirubin:- Negative
Ketones:- Negative
Nitrates :- Negative
Pus cells:- 5-6 /HPF
Rbc:- 5-7 /HPF
Epithelial cells:- 1-2/HPF
Casts:- Granular casts present
Crystals :- Nil
2D echo :-
Impression -
EF:- 48%
Dilated LA
Conc LVH
Moderate MR/ Mild AR / Mild TR
No PAH/ No PE/ No CLOT
No RWMA
Sclerotic AV .
CT KUB : showing left kidney 7-8 cm Staghorn calculus causing mild hydronephrosis and thining of parenchyma
Ascitic fluid analysis showed - HIGH SAAG
Examination videos links :
Final diagnosis -
Ascitis secondary to portal hypertension - ? Post hepatic -
Secondary to Congestive cardiac failure (HFPEF)
Post renal AKI on CKD - Left staghorn calculus
CKD - Stage 5 - Native kidney disease - ? Htn nephropathy
Cardio- renal syndrome type 4
-----------------------------------------------------------------------------------------------------------------------------
CRITICAL APPRAISAL:
Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction .
RCT - placebo control trial .
https://www.nejm.org/doi/full/10.1056/NEJMoa1911303.
P- Total 4744 patients with HFref .
2373- Dapagliflozin 10mg od .
2371 - placebo
I- Dapagliflozin vs placebo
C- Placebo
O - The primary outcome was a composite of worsening heart failure (hospitalization or an urgent visit resulting in intravenous therapy for heart failure) or cardiovascular death.
1) 237 - In dapaglifozin grp had worsening heart failure and 227- Died.
2) 326- placebo had worsening HF
273- DIED .
CONCLUSION :
Among patients with heart failure and a reduced ejection fraction, the risk of worsening heart failure or death from cardiovascular causes was lower among those who received dapagliflozin than among those who received placebo, regardless of the presence or absence of diabetes.
But pts who were included , dapagliflozin had more patients with NYHA class 2 and placebo had more pts with NYHA class 3,4 HF . Which can explain frequent hospital admissions in them .
More larger data is required and they dint mention about what happened to other remaining patients .
And also all the patients received ARNI/ARB and beta blockers along with SGLT2 OR Placebo.
So individual benefits couldn't be estimated .
But according to numbers they showed ,lesser hosp admissions and mortality was there for SLGT-2 group .
LIMITATIONS :
This trial has some limitations. We used specific inclusion and exclusion criteria, which may have limited the generalizability of our findings.
The baseline use of sacubitril–valsartan, which is more effective than renin–angiotensin system blockade alone at reducing the incidence of hospitalization for heart failure and death from cardiovascular causes, was low.






























































































Comments
Post a Comment