19100006007 CASE PRESENTATIONS
LONG CASE :
50 year old male, working as a mason for past 25 years, who is staying away from his family to fetch a livelihood started to experience detoriation in his health from past 5 months, where in patient developed fever, which is continuous, aggravating in evenings associated with chills and relieved with night sweats. Patient also started having complaints of cough, which was characteristically exhaustive to the tune that patient some times use to gasp for breath. Cough is productive with copious amount and mucoid consistency. Patient use to take symptomatic medications untill he had come for his daughters marriage 2 months back, after which the family members took him to hospital where he was treated with IV Antibiotics symptoms subsided only to recur with in a span of one to two weeks.
The attenders observed there was a marked decrease in appetite with comprehensive reduction in carbohydrate & protein content of his diet which was differing from his previous diet. There was an association of weight loss also, to which objectively patient confirms he lost 14kgs in last three months. On persistence of symptoms with the backdrop of this clinical picture patient was tested for Retroviral disease which turns out to be positive. Patient was started on ART ( Triple drug regime ).
Later on from last 15 days patient experiencing pain abdomen localised to peri umbilical region with single swelling in the posterior triangle of neck which is rubbery in consistency freely mobile not fixed to underlying structures measuring about 2 X 1 cms in size.
Past History
Personal History
Family History
Social History
Problem representation :
50/M construction worker with known retroviral disease (HIV-1) now has a foreground of cough with copious expectoration, fever, drenching night sweats and weight loss with loss of appetite.
The collective syndrome of fever with cough and sputum localises it to the respiratory tract. The symptom of copious mucoid sputum suggests that there is mucus glands hypersecretion due to inflammation.
Cachexia is indicative of chronic systemic inflammation and is also supported by involuntary weight loss, eq r muscle and fat tissue and an elevated BMR.
The presence of abdominal and neck swellings are suggestive of lymph nodes. The presence of lymph nodes on both sides of the diaphragm indicates generalised lymphadenopathy
Provisional Diagnosis :
RETROVIRAL DISEASE WITH ?AIDS DEFINING ILLNESS ( ExtraPulmonary Tuberculosis / Lymphoma ).
Clinical Examination
General Examination
Systemic Examination
Lymphatic system
On inspection : found to have globose swelling measuring 2 X 1 cm in the posterior triangle of neck on the right side, no scars & discharging sinuses, no discolouration of the skin over the swelling.
Palpation : inspectory findings are confirmed on palpation of cervical group of lymph nodes.
On Palpation multiple small lymph nodes felt over the periumbilical area of the abdomen.
2 X 2 cm swelling felt in the left inguinal area.
No gross swellings observed in axillary and popliteal area.
Labs indicate a normocytic anemia and a borderline low TLC count which could suggest a bicytopenia.
The low TLC count could suggest depressed bone marrow function or bone marrow infiltration.
The CD4 count and the positive HIV test confirm chronic secondary T cell mediated immunodeficiency due to HIV, in immunological and suspected clinical failure.
Summary
50/M with immunological and clinical failure of suppression of HIV has a 3 month history of new onset systemic inflammation localising to lungs and lymph nodes.
Functional Problem - Cough, expectoration, cachexia
Anatomical Problem - Larger airways (bronchiectasis strong possibility) and lymph nodes.
Pathology - Inflammation
Etology - Infections - TB (most likely) NTM, HIV-2 Co infection, Brucellosis.
Malignancies - Non Hodgkins Lymphoma - DLBCL, Multicentric Castleman's Disease, Hodgkins Lymphoma (less likely)
Autoimmune - Sarcoidosis,
Drugs - Unlikely.
A 62 yr old female, home maker by occupation presented to OPD with the
Chief complaints of
-Shortness of breath on exertion since 5 days
-Bilateral lower limb swelling since 5 days
-Decreased urine output which was worsening since 5 days
The above chief complaints were gradually progressive from last one year and patient had debilitating effects from last one week.
HISTORY OF PRESENTING ILLNESS :
Patient was apparently asymptomatic 20 years back , was diagnosed to be diabetic incidentally on routine workup an an instance of fever and was started on oral hypoglycaemic agents on TAB.GLIMI2
1990 :
She underwent tubectomy
2002 :
Pt developed pain abdomen for which pt was admitted in hospital and undergone HYSTERECTOMY ?FIBROIDS .
2009:
Pt developed chest pain for which he was admitted in hospital and she was taken for primary PTCA.
On angiogram it was showing a double vessel disease (RCA+ LAD)
Since 2009 she had intermittent episodes of pain abdomen in epigastric region which was relieved on medication with PPI.
2012
Underwent cataract surgery in two eyes with 6 months interval
2016:
She had another episode of chest pain she was taken to hospital and was taken for primary PTCA to LAD ?stent thrombosis.
Around 2021 :
She developed bilateral pedal oedema associated with decreased urine output ,shortness of breath was diagnosed to be having a renal disease and was started on medication accordingly and continued to use OHA’s intermittently with insulin and stopped using because of poor compliance.
Pt had an episode of sweating, palpitations with slurring of speech and deviation of angle of mouth followed by unresponsiveness, her GRBS was 35mg/dl. MRI brain was done showing no structural lesions, and was diagnosed to be hypoglycemic seizure episode (sweating, slurred speech, deviation of mouth and unresponsiveness) and the symptoms reverted after correction of hypoglycaemia, this episode was attributed to the change in her dosage and timing of OHA’s.
She had similar history of developing pedal oedema on and off with decreased urine output and shortness of breath 5 months back. Patient was evaluated and was found to have anemia which was managed by systemic iron therapy.
From the past one month patient started experiencing, nausea, vomiting, loss of appetite and dyspepsia.
Presently admitted for similar complaints.
General examination:
Patient is conscious, coherent, co-operative, oriented to time, place and person.
No Icterus, Cyanosis, Lymphadenopathy,
Pallor ++
B/l pitting type Edema +
B/L pedal edema
Vitals:
Bp: 100/70mmHg
PR: 96bpm
SpO2: 98%@RA
Temperature:98. 6°F
GRBS: 102 mg/dl
SYSTEMIC EXAMINATION :
CARDIOVASCULAR SYSTEM :
S1, S2 +, mid diastolic murmur in Tricuspid and mitral area.
Apex beat in 5th ICS on the MCL.
JVP normal.
RESPIRATORY SYSTEM :
Shape & symmetry of chest - Normal
Respiratory movements - Equal on both sides
BAE+
NVBS
Abdominal Examination
Soft, Non-tender
No organomegaly
Bowel sounds+
CNS :
Higher Mental Functions : intact
Cranial nerve Examination : no abnormality detected.
MOTOR SYSTEM
Right. Left
Bulk Normal Normal
Tone Right Left
Upper limb Normal Normal
Lower limb Normal Normal
✓Power
UL
Proximal 5/5 5/5
Distal 5/5 5/5
LL
Proximal 5/5 5/5
Distal 5/5 5/5
✓Reflexes
Superficial reflexes
Right Left
Plantar - -
Deep tendon reflexes
Right Left
Biceps 2+ 2+
Triceps 2+ 1+
Supinator 1+ Absent
Knee 2+ 2+
Ankle 1+ 1+
✓SENSORY SYSTEM
Right Left
Pain + +
Fine touch + +
Temperature + +
Vibration Intact Intact
Proprioception Intact Intact
Stereognosis Normal Normal
Gait - Normal
CEREBELLUM FUNCTIONS : Intact.
AUTONOMIC
No postural hypotension.
No urinary urgency, frequency, hesitancy.
No diaphoresis.
INVESTIGATIONS:
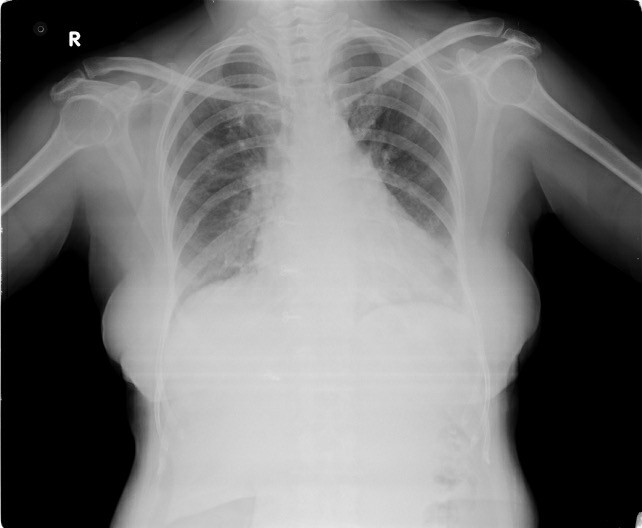
Chest xray -Pa view
ECG:
USG ABDOMEN :
Diagnosis:
ANEMIA SECONDARY TO CHRONIC KIDNEY DISEASE
? DIABETIC NEPHROPATHY
S/P:OLD CAD -PTCA +DES TO LAD (2009 ,2016)
WITH TYPE -2 DM SINCE 20 YEARS
---------------------------------------------------------------------------------------------------
SHORT CASE 2:
A 47 year male patient came with chief complaints of abdominal distension and swelling of bilateral lower limbs since 6 months which is gradually increasing since 10 days and and fever since 2 days.
History of present illness
Patient was apparently asymptomatic 18 months back then he noticed abdominal distension which is insidious in onset and gradually progressive in nature and subsequently noticed bilateral swelling of lower limbs , he was hospitalized for one week and took medication which increased his urine output and abdominal paracentesis was done and felt better ,, However he discontinued medicine 6 months back and presented with similar complaints where he was hospitalized and treated conservatively , he was hospitalized 3 months back again with similar complaints , again abdominal paracentesis of 1.5 to 2 lit was done. He is on medication , the past 10 days he noticed abdominal distension associated with swelling of bilateral lower limbs which started at ankle and progressed upto knee
H/0 of fever, low grade,intermittent in nature not associated with chills, since 2 days,
H/0 of anorexia, fatigue and generalized weakness since 3 months,,
H/0 of disturbed sleep since one month, where he complained of excessive day time sleepiness and night distured sleep,
H/0 of yellowish discoloration of eyes 3 months back now it subsided,
No h/0 of nausea and vomitings,
No h/0 of pain abdomen
No h/0 of decreased urine output
No h/0 of high coloured urine and clay coloured stools.
No history of shortness of breath
No history of blood transfusions
Past medical illness-
History of abdominal distension , swelling of bilateral pedal oedema, and hematemesis one episode 50 ml 18 months back ,where he admitted in an hospital for 10 days which relieved with diuretics , abdominal paracentesis and gastric oesophageal ligation was done.
Appendicectomy 25 years ago
No history of hypertension, diabetes, thyroid , epilepsy or seizure disorder.
Personal history-
Diet - mixed
Sleep - disturbed , excessive day time sleep , night time disturbed sleep since one month.
Appetite- decreased.
Bladder habits- regular and normal.
Habits- chronic consumption of alcohol since 20 years daily , country liquor of 500 ml nearly 110gm per day, and whisky of 150 ml per day nearly 50gm per day,
Last binge of alcohol - 3 days before admission he took 100gm.
Summary - Decompensated chronic liver disease secondary to ethanol consumption, with ascites, portal hypertension, hepatic encephalopathy stage 1 and spontaneous bacterial peritonitis.
General examination -
Moderately built and nourished.
Patient is oriented to time , place and person.
GCS - E4 V5 M6
VITALS -
Pulse - 82 beats per minute, regular normal volume ,and character, no radio radial or radio femoral delay.
Blood pressure - 100/70 mm Hg, right arm supine position.
Respiratory rate - 18 cpm, thoracoabdominal.
Spo2- 98 % on room air
Jvp - not elevated.
Physical examination-
pallor - present
Icterus - absent
No cyanosis
No clubbing
No generalized lymphadenopathy
Pedal edema +
Head to toe examination-
Axillary and public hair - sparse.
B/ l parotid enlargement - negative
No fetor hepaticus
No asterixis
No gynaecomastia
Spider nevi - absent
No planar erythema
No leuconchyia
Inspection -
Oral cavity - No dental caries and no Tobacco staining
Abdomen - flanks full, distension.
Appendicectomy scar present.
Distened veins present.
No visible peristalsis or no visible pulsations.
Palpation -
Done in supine position with Both Limbs flexed and hands by side of body.
No tenderness or local rise of temperature.
Abdomen - soft.
No gaurding and rigidity
Hepatomegaly present
Spleen not palpable
Kidneys bimanually palpable , ballotable.
Fluid thrill - present
Abdominal girth - 98 cms .
Xiphisternum to umbilicus - 16 cms
Public symphysis to umbilicus - 13cms
Percussion -
Liver span - 15.7 cm in mid-clavicular line
Auscultation :
Normal bowel sounds heard.
No hepatic bruit , venous hum or friction rub.
Examination of external genitilia - No testicular atrophy.
Examination of spine - Normal.
Provisional diagnosis -
Decompensated chronic liver disease
Etiology - chronic ethanol related.
Ascites , Hepatic encephalopathy grade 1
Esophageal gastric ligation bands were.
Child-Pugh SCORE - C
MELD SCORE - 9
Investigations-
CBP -
HB - 7.3
TLC - 9600
PLT - 1.97 LAKH
CUE -
Albumin- trace
Sugar- nil
Rbcs- nil
Pus cells - 2 to 3
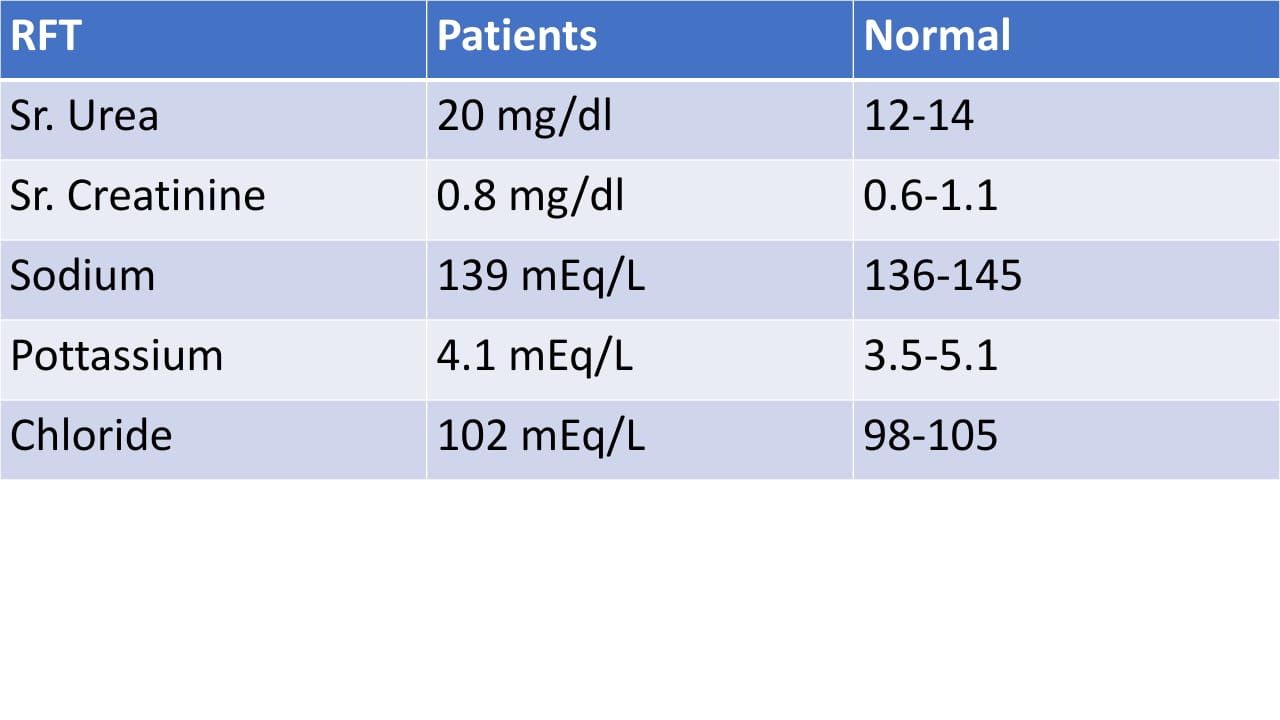
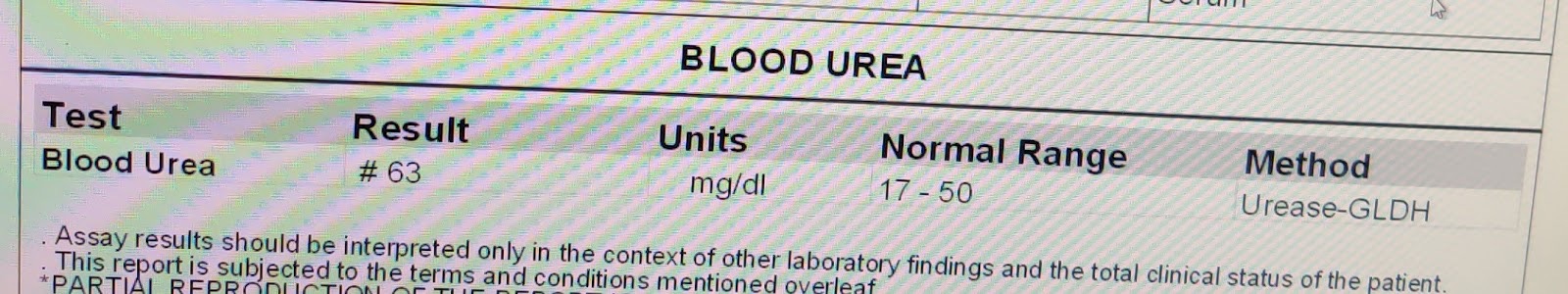
RFT -
Blood urea - 12mg/ dl
Serum creatinine - 0.7mg/dl
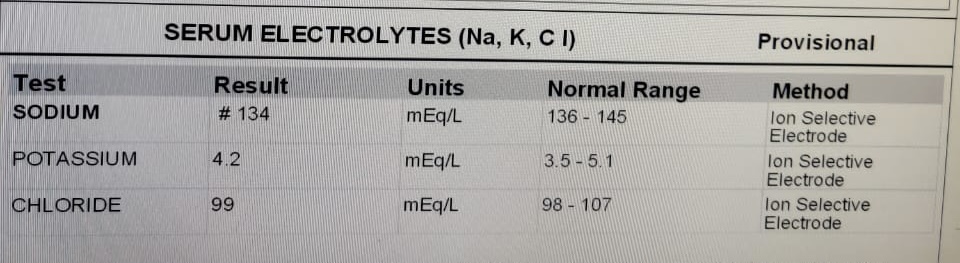
Sodium - 139 meq/l
Potassium - 3.4meq/l
Chloride - 99 meq/l
Uric acid - 5.0
Calcium - 9.1
Phosphorus - 7.0
LFT -
Total bilirubin - 10.46 mg/ dl
Direct bilirubin - 8.84mg/dl
SGOT - 140IU/L
SGPT - 17 IU/L
ALP - 321 IU/L
Total protein - 6.9gm/dl
Albumin - 2.2 gm/ dl
RBS- 70mg/dl
Ascitic fluid analysis -
SAAG - 1.85. Serumalbumin - 2.2
Ascitic albumin - 0.35
Ascitic LDH - 38 IU/ L
Ascitic sugar - 126mg/ dl
Ascitic protein - 0.8 g/dl
Appearance - Clear
Total count: 50 cells
DLC:80% neutrophils
20% lymphocytes
RBCS - nil
Impression: Negative for malignancy
PT - 18 Sec.
APTT - 35sec.
INR - 1.33
BGT AB+
Hiv - negative.
Hbsag -negative.
Hcv - negative
CHEST X-RAY AP VIEW
---------------------------------------------------------------------------------------------------
CRITICAL APPRAISAL:
Utility of CBNAAT, Cytology and Histology in diagnosis of suspected tubercular solid lymph node
Aims and Objectives:
To asses efficacy of various diagnostic tools for diagnosis of lymph node tuberculosis in solid state (non-caseating stage).
Methods :
Prospective observational study over a period of 18 months
Inclusion criteria :
Clinically suspected extra Pulmonary TB
Suspected LNTB patients on ATT
Exclusion criteria :
HIV positive patients
Fluctuant node
on ATT
Patients with cheesy / pus on aspiration of node.
Patients :
82 patients were initially selected out of which 22 patients were excluded from the study as they are under exclusion criteria.
Out of 60 patients 31 ( 51.67%) were tested positive for MTB in CBNAAT of which 2 are Rifampcin Resistant and remaining 29 patients were opted for excisional biopsy.
Remaining patients after histology had following diagnosis; Tuberculosis in eight, nonspecific reactive hyperplasia in 11, metastasis and lymphoma in four and Non Tubercular Mycobacteria and actinomycosis in one each patient.
9 out of 60 ( 15%) were detected AFB on ZN stain of which all are CBNAAT positive for MTB.
CBNAAT could not diagnose (8/39) 20% of patients with tuberculosis which are diagnosed by histopathology.
CBNAAT diagnosed 22 (70%) cases which were missed by AFB smear & 16 cases missed by cytology.
Cytological findings of tuberculosis -granulomatous inflammation with or without necrosis was looked for and found in 21/60 patients
A peculiar pattern of reactive hyperplasia was found in 26/60 out of which 15 found positive for MTb on Cbnaat or histology.
Cytological finding correlated with final diagnosis (including Tuberculosis and other diagnoses) in 56.67 % (34/60) cases and final diagnosis was different from cytology in 43.33 % (26/60) cases.
Conclusion :
CBNAAT has 79% sensitivity ( ruling out a disease ) and 100% specificity ( ruling in a disease) in diagnosing Lymphnode Tuberculosis even in adinitis and non caseous stage although yeild is less compared to caseous stage.






































Comments
Post a Comment