19100006008 CASE PRESENTATION
LONG CASE :
50 years old male, who is agricultural farmer by occupation, presented to casuality on 19/5/22 with complaints of
c/o altered level of consciousness ( drowsiness) since 19/5/22 morning
c/o vomitings since 4 days
c/o burning micturition since one week
c/o fever with chills since 2 days
HOPI-
pt wife- daily labourer
patient was apparently asymptomatic one week back, he was complaining of burning sensation while urinating since one week with increased frequency, later he had vomitings 4-6 episodes per day,associated with nausea, contains food particles, non blood stinged,non bile stained, for about 4 days which subsided on taking medication( brought from local pharmacy).
c/o fever sudden in onset, associated with chills, associated with sweatings, intermittent type, high grade since 2 days.
patient attenders noticed , slurring of speech and in drowsiness state, not responding to oral commands on 19/5/22 since morning which made them bring to the hospital.
no h/o pain abdomen, constipation,diarrhoea.
no h/o cough,cold, headache
no h/o weakness of bilateral upper and lowerlimbs
no h/o chestpain, syncopal attacks
no h/o trauma
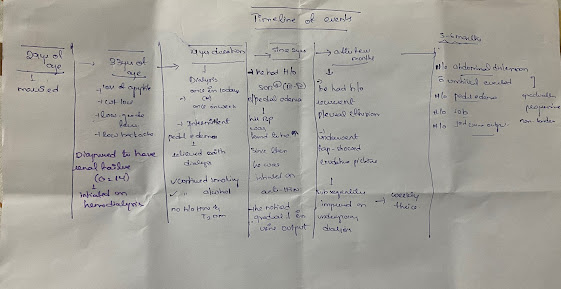
Time line of events -
h/o increased frequency of urination and urgency.
personal history:
decreased appetite (mixed diet)
chronic alcoholic since age of 20 years
chronic smoker (daily 5-6 chuttas per day)
bowel and bladder movements regular with increased frequency and burning micturition present.
PROVISIONAL DIAGNOSIS:
Altered sensorium under evaluation ( secondary to ? septic encephalopathy)
Fever under evaluation ( secondary to ? UTI)
H/o type2 diabetes mellitus.
GENERAL EXAMINATION:-
On day of admission pt is in irritable state and not oriented to time place person
GCS- E4 V2 M5
Moderately built, moderately nourished
pallor - present
no icterus, cyanosis, lymphadenopathy, grade 2 clubbing present
mild pedal edema pitting type up to ankle present.
Vitals on admission-
Temperature: 101F
BP: 110/80 mmhg
PR: 98bpm
RR: 22cpm
Spo2 : 98% on RA
GRBS: 250 mg/dl
SYSTEMIC EXAMINATION-
GASTROINTESTINAL SYSTEM:
inspection- soft, generalised distended abdomen , normal and inverted umblicus
no visible pulsations, mass, dilated veins, scars or sinuses
palpation- tenderness present at rt loin region( noticed as patient winced on palpation)
no local rise of temperature
no palpable liver and spleen
percussion- no shifting dullness
normal liver span
ascultation- bowel sounds present
CENTRAL NERVOUS SYSTEM:
Pt is conscious, irritable, not oriented to time place and person
slurring of speech present
Pupils normal in size , b/l reacting to light
motor system -
tone rt lt
UL N N
LL - N
reflexes rt lt
superficial reflexes
corneal + +
conjuctival + +
plantars flexors
deep tendon reflexes
biceps - -
triceps - -
supinator - -
knee - -
ankle -
no neck stiffness, no kernigs and brudzinski sign.
RESPIRATORY SYSTEM:
normal vesicular breath sounds heard, no added sounds
CARDIOVASCULAR SYSTEM:
s1s2 heard.
no murmurs heard.
Investigations:
hemogram-
hb: 8.0, tlc: 22900, pcv: 21.6,mcv: 73.5, mch: 27.2, mchc : 37.0 plt : 1.50
smear- normocytic hypochromic, neutrophilic leucocytosis.
cue:
albumin- 4+, sugar- nil, pus cells- plenty, epithelial cells- 3-4, rbc- 2-3, casts- nill, bacteria present
urea-129, creatinine- 4.5,uricacid- 7.7, calcium-9.9, phosphorous- 2.0, na- 124, k- 2.6, cl-90
Lft:
tb- 1.52, db- 0.50, ast- 21,alt- 10,alp-275, tp- 5.6, albumin-2.3, a/g ratio- 0.72
abg:
ph- 7.2, pco2-32, hco3- 17,o2sat- 96%
serology( hiv.hbsag,hcv- negative)
spot urine protein creatinine ratio- 5.62
24hrs urinary protein- 434.2
PT- 18, INR- 1.3, aPTT- 35
urine c/s sent showed- plenty of pus cells seen, klebsiella pneumonia isolated
blood c/s sent showed - klebsiella pneumonia isolated.
usg abdomen- ? rt sided kidney emphysematous pyleonephritis, lt sided kidney subcapsular collection noted.
chronic pancreatitis
plain xray kub-
chestxray-
ecg-
course of events:
pt was started on
inj meropenem 500mg iv bd
inj zofer 4mg iv bd
iv fluids ns rl @ 100ml/hr
inh H. actrapid sc tid after checking grbs.
tab pcm 650mg po sos
temp charting 4th hrly and tepid sponging
i/o charting and grbs charting
on day 2 (20/5)
pt sensorium improved, conscious,drowsy, oriented to person not to time place
fever spikes +
burning micturition+
vomitings +
planned for ncct kub showed-
rt side emphysematous pyelonephritis ( renal parenchyma, renal pelvis,urinary bladder with perinephric fat stranding and fluid.
lt side subcapsular collection in upper and mid pole ( 15mm thickness) ( early pyelonephritis)
chronic pancreatitis
.jpeg)
pt underwent b/l DJ stenting on 25/5. and planned for percutaneous nephrostomy.
pt is drowsy, conscious, oriented to place person not to time,
tlc count is in increasing range , with intermittent fever spikes and also noticed fall in platelet count from 1lakh to 7000.
Final diagnosis:
rt sided kidney emphysematous pyelonephritis
lt sided kidney acute pyelonephritis
septic encephalopathy( resolving)
acute kidney injury secondary to sepsis
anemia ( normocytic,normochromic) secondary to ? chronic inflammation.
thromboctopenia secondary to ?sepsis.
h/o type2 diabetes mellitus.
Discussion:
nnalsofintensivecare.springeropen.com/articles/10.1186/s13613-017-0337-7
https://www.sciencedirect.com/science/article/abs/pii/S2387020621000528
---------------------------------------------------------------------------------------------------
SHORT CASE 1:
23 years young female daily labourer by occupation presented to opd with chief complaints of
c/o shortness of breath on exertion since 5 days
c/o generalised weakness of body since 5 days
HOPI:
Time line of events-
on april 2021, visited gynic opd,in view of excessive menstrual bleeding. her hb-10.9,plbs- 179,hba1c-6.4, thyroid profile- normal, usg abdomen- grade1 fatty liver. adviced wt reduction , oral iron tablets
on may 2021 visited endocrinology opd, wt 105kg, ht 153cms, BMI- 41.6, ( obesity), adviced lifestyle modifications and physical activity.
next visit on july 2021, then her bp -150/80 mmhg,fbs -114,plbs- 167, hba1c- 6.4, adviced diabetic diet with small frequent meals, and physical activity.
thereafter not on follow up.
now she presented with c/o shortness of breath, sudden in onset intially on exertion now even while going to washroom she c/o sob since 5 days, associated with orthopnea .
H/o generalised weakness of body, and easily getting tried with minimal work unable to perform her household activities.
h/o swelling of b/l lower limbs pitting type up to feet region.
no h/o chestpain, palpitations,giddiness, syncopal attacks
no h/o fever,cough,cold
no h/o altered bladder and bowel habits.
no h/o pain abdomen.
PERSONAL HISTORY-
takes mixed diet: morning- either tea or coffee
lunch- one cup of rice with either vegetable curry or dal
dinner - follows the same.
no addiction habits
normal bladder and bowel movements
h/o weight gain
adequate sleep pattern
FAMILY HISTORY-
nil significant.
PROVISIONAL DIAGNOSIS-
Dyspnea under evaluation secondary to ? heart failure
obesity
?anemia secondary to menorhagia
GENERAL EXAMINATION -
pt is conscious, coherent, cooperative
wt- 115kg, ht- 153cms, BMI- 49.1 kg/m2
waist circumference- 121 cm
pallor +, no icterus,cyanosis, clubbing, lymphadenopathy.
mild b/l pedal edema +, pitting type up to feet region.
vitals on admission:
temp- 98.6f
BP- 160/100 mmhg
PR- 94 bpm
RR- 20cpm
Spo2- 97% at room air
Grbs- 140 mg/dl
JVP - elevated
HEAD TO TOE EXAMINATION-
acanthosis nigricans present
no skin tags, xanthelasma
no facial hair
axillary and pubic hair present
thyroid - no goitre noted
no purple striae over abdomen
SYSTEMIC EXAMINATION-
CARDIOVASCULAR SYSTEM-
Inspection - normal chest shape and bilaterally symmetrical
no visible pulsations
palpation - apical impulse felt at 5th intercoastal space medial to midclavicular line
no papable parasternal impulse, thrills
ascultation- s1 s2 heard
RESPIRATORY SYSTEM-
normal vesicular breath sounds heard, no added sounds
PER ABDOMEN-
obese, soft, no palpable organomegaly
bowel sounds present
CNS-
no focal neurological defecit.
Investigation-
hemogram:
hb- 7.1 ,tlc-12,600, mcv- 61.8, mch- 17.8, mchc- 28.9, plt- 3.52
smear- microcytic hypochromic anemia
sr ferritin- 6.9
retic count- 1.1. absolute retic count- 0.6
abg:
ph- 7.42, pco2- 29.4, po2- 71.5, hco3- 19, o2 sat- 94%
urea-25,cr- 0.9, na-140,k- 3,7, cl- 98
tb- 0.62, db-0.20,alb- 3.2
cue:
alb- nil, sugars- nil, puscells- 2-4
hba1c- 6.4 ,fbs- 152 plbs- 180
fasting lipid profile-
tc- 120, tg- 150, hdl- 35, ldl- 80
thyroid profile- normal
usg abdomen- grade 1 fatty liver
2D ECHO:
Dilated right atrium, mild TR,PAH( RVSP= 50mmhg)
No RWMA, EF- 62%, IVC -dilated
Good LV systolic function
Final diagnosis:
Iron deficiency anemia ( microcytic hypochromic) secondary to mennorhagia
Metabolic syndrome secondary to obesity
Right heart failure
h/o diabetes and hypertension
--------------------------------------------------------------------------
SHORT CASE 2:
39yr old male , who used to runs his own xerox centre, married 10yrs ago, currently he is having complaints of
Abdominal distension since 6months
B/l swelling of lower limbs since 6months
Married. Has a healthy daughter with age of 10yrs.
He was apparently asymptomatic 6yrs back.
His daily routine was, he used to wake up around 7, undergo his daily natural activites, goes to xerox centre around 10, comes to house for lunch in the afternoon, goes back to work again.
In the evening times with his friends around his house, consumes alcohol around 250ml a day whiskey.
Smokes around 20-30cigarretes per day.
Currently he is not working and stays at home.
6yrs back he intially noticed decreased appetite, weight loss( loosening of his clothes), intermittent low grade fever (relieved on taking paracetamol) and low back ache he visited local RMP took pain killers for relief of symptoms (for about 1month)..
As his symptoms are persistent he visited a hospital near by his location and underwent routine blood tests and his sr creatinine was found to be high (11) and referred to our centre.
At our centre, his creatinine was (14), and his kidneys were bilaterally small in size and initiated on hemodialysis.. (? The cause of renal failure).
After one month of initiation of dialysis he undergone AV fistula ( lt forearm).. since for about 4years he used to get dialysis once in ten days/ once in week ..
He had intermittent pedal edema which relieved on dialysis.. but he didn’t notice any symptoms of sob, decreased urine output in past 4years..continued to have 10-15 cigarettes perday, alcohol 180ml once in a week.
Time line of events:-
HAS BEEN ON DIALYSIS SINCE 6YRS.
H/O alcohol since 20yrs, every alternate day around whiskey 200ml/day. Now since 2-3yrs he stopped consuming alcohol.
He is a smoker since 20yrs, smokes around 20-30 cigarettes per day, before 6yrs.
NOW HE SMOKES AROUND 10-12 CINGARETES PER DAY
No H/O DM, EPILEPSY, THYROID, TB ASTHMA.
No significant family history.
On general examination:-
Pt was conscious, coherent, cooperative
Pallor+, no icterus,cyanosis, clubbing present, no lymphadenopathy, pedal edema present
Moderately built, moderately nourished
Respiratory system- b/l air entry present, normal vesicular breath sounds heard.
cardiovascular -
inspection- b/l chest symmetrical,
raised jvp
apical pulse - visible
palpation-
apical pulse palpable at lt 6th intercoastal space lateral to midclavicular line,
parasternal heave - grade 2
ascultation - s1 s2 heard
GIT- distended with flanks full, umbilicus everted
no dilated veins
non tender, fluid thrill present
bowel sounds heard
CNS- no focal neurological defecit.
INVESTIGATIONS-
cbp- normocytic normochromic anemia
lft- tb- 1.09,db-0.30, ast-15,alt11, alp- 720,tp-6.7, sr alb- 3
rft- urea-90, cr- 5, na- 139,k -4, cl-97
cue- 2+ albumin, sugars- nil, no casts
Ascitic fluid analysis-
High SAAG(1.6) Ascitic protein - 3.7
USG abdomen- B/l grade 3 RPD changes with decreased size, gross ascites+
c-xray:
ECG-
Final diagnosis:
Chronic renal failure(? cause) on maintainence hemodialysis
Heart failure with preserved ejection fraction (type4 chronic renocardiac)
Ascites secondary to ? heart failure
Anemia of chronic kidney disease
h/0 hypertension ( ? secondary to ckd)
Discussion:
what could be the risk factors for occurence of ckd in this patient?
risk factors-
Htn in ckd
cause of ascites in this patient could be secondary to post hepatic portal hypertension ( heart failure).
smoking also contributes for the progression of renal disease as it:
it thickenes and hardening of the renal arteries
reduces blood flow to kidneys
narrows the blood vessels in the kidney
increases blood pressure
------------------------------------------------------------------------------------------------
CRITICAL APPRAISAL:
A Randomized Clinical Trial of Insulin Glargine and Aspart, Compared to NPH and Regular Insulin in Children with Type 1 Diabetes Mellitus .
P -Forty patients with T1DM were enrolled in this study. During run-in, all subjects were treated with conventional therapy consisting of twice-daily NPH and thrice-daily regular. Following randomization, 20 subjects received Glargine and Aspart and 20 subjects received NPH and Regular insulin.
I - Glargine and aspart ( 20 patients) .
C- regular and NPH( 20 patients)
O -Mean HbA1c was 8.8% and 8.6% at first and 8.4% and 8.2% at the end of study for subjects randomized initially to Glargine and Aspart and for those randomized to NPH and Regular, respectively (P>0.05).
Mean fasting blood glucose (FBS) of the subjects randomized initially to Glargine and Aspart was 217±101 mg/dL, with no significant difference to 196±75 mg/dL for those randomized to NPH and Regular. At the end of the study, mean FBS was 169±55 mg/dL with Glargine and Aspart as compared to 173±2 mg/dL with NPH and regular (P=0.48).
The overall frequency of hypoglycemia during treatment in both groups was decreased significantly (Before treatment with Glargine and Aspart: 4 episodes of moderate hypoglycemia in 3 patients and 2 episodes in 2 patients in Group 1, while 3 episodes in 5 patients in Group 2; after treatment with Glargine and Aspart: 1 episode in 2 patients in postprandial state in Group 1 and 2 episodes in 2 patients and 1 episode in 3 patients in Group 2).
but the difference was not significant (P=0.39).
The current study showed no significant difference in glycemic control [Glycated hemoglobin (HbA1c) and FBS] and lipid profile (total cholesterol; p=1, and triglyceride; p=0.36) between two regimes.
.png)
.png)







.jpeg)
.jpeg)
.jpeg)
.jpeg)
.jpeg)


.png)
.png)
.jpeg)
.jpeg)
.jpeg)

.jpeg)
.jpeg)











Comments
Post a Comment