19100006010 CASE PRESENTATION
LONG CASE:
A 30 year old man who is an electrician by occupation came with complaints of
Sudden onset weakness of right upper limb and right lower limb 2 days back
Deviation of mouth to left side since 2 days
History of present illness:
Patient was apparantly asymptomatic 2 days back then he developed weakness of right upper limb and right lower limb which was sudden in onset associated with deviation of mouth to left side and slurring of speech.
Weakness was predominantly on right arm than right leg.
There was no diurnal variation of weakness and
No history of wasting or thinning of muscles
No history of pain or muscle cramps or fasiculations and any involuntary movements
No history of tingling , numbness or any pricking like sensation.
No history of loss of consciousness or alteration in sensorium or any bowel bladder involvement. And speech aphasic.
No history of alteration of smell, blurring of vision, diplopia, dysphagia.
Frowning and ability to close eyelids present.
No history of giddiness, syncope , sweating or palpitations
No history of fever ,headache ,vomiting, neck stiffness.
No history of trauma , fall from height or any drug intake.
Past history:
No history of similar complaints in the past.
No comorbid illness like Diabtes Mellitus , Hypertension, coronary artery disease, thyroid disease,HIV,Tuberculosis,malignancy,surgeries.
Personal history:
Married And Non vegetarian with normal sleep and appetite.
No alcohol and smoking habits.
Family history:
Non consanguinous marriage ,With no similar complaints in the family.
No significant past treatment history.
Summary:
Onset - Acute
Progression - rapidly progressive
Neurological - hemiparesis with UMN type fascial Nerve involvement
Anatomical - cortex>subcortical
Etiology - secondary to vascular or inflammatory.
General examination
Patient conscious and oriented to time place person
Moderately built and nourished
Afebrile
No pallor, icterus, clubbing, koilonchia, lymhedema and pedal edema.
Temperature : Afebrile
PR : 78 bpm, regular , normal in volume and character with no radio radial delay or radio femoral delay.
BP: 130/80 mm hg in right and left arms.
RR: 16 cpm
No cerebellar signs.
Cardiovascular system:
S1,S2 heard and No thrills or murmurs
Respiratory system:
Bilateral air entry and Normal vesicular breath sounds heard.
Per abdomen:
Soft and no organomegaly
Provisional diagnosis : Cerebrovascular accident : Acute Right sided hemiparesis with Right UMN type of fascial Palsy with Broca's aphasia with subcortical (frontal and parietal lobe, temporal) infarct involving MCA territory
Investigations:
Hemogram : Hb :14.4 gm/dl
Tlc :7,200 cells/cumm.
Platelet : 2.69 lakhs/cumm
RBS : 101mg/dl
LFT :
Total bilirubin: 1.02 mg/dl
Indirect bilirubin : 0.19
Total proteins:7.45
Albumin: 3.9
RFT :
serum creatinine 0.9
Serum electrolytes normal
Fasting lipid profile :normal
ESR : 20mm/hr
CRP : negative
D Dimer : 300 ug
RA factor: negative
HIV : Non Reactive
HbsAg: Non reactive
VDRL : Negative
ECG
 |
12 lead ECG at 25 mm/sec showing sinus rhythm with regular RR interval with normal p wave QRS complex and T wave morphology
C-xray :
C-xray PA view inspiratory and non rotated film.
Domes of Diaphragm clearly seen and well defined with no cardiomegaly
Right heart border and left heart border are clear with no Hilar lymphadenopathy or any Lymph node enlargement.
Bones and ribs appear normal.
MRI brain :
This is a T2 Flair image showing hyperintesity in the left frontal and parietal region suggesting an acute infarct.
2decho: Normal LV systolic function
No regional wall motion abnormalities
EF : 58%
Treatment:
Tab Ecospirin AV 75/20 OD
Tab Clopidogrel 75 mg OD
Tab Pantop 40 mg OD
Tab Supradyn OD
Physiotherapy of right upper limb and lower limb.
Discussion:
Ischaemic stroke in young:
Definition : Many authors consider age of 45 years as upper limit for stroke in young.
Epidemiology: About 10-15% of total number of strokes occur in younger patients which constitute approximately 2 million adolescents and young adults across the world suffer from an ischaemic stroke.
Risk factors :
Conventional risk factors like Diabetes Mellitus, Hypertension, dyslipidaemia.
Risk factors for stroke in young include smoking , alcohol, drug abuse: cocaine IV drug users and oral contraceptive pills.
Migraine with aura , Malignancy
Etiology:
1)Cardiac causes:
30% of stroke in young is secondary to cardiac cause: Congenital heart disease , PFO,
Atrial fibrillation , Acute MI, cardiomyopathy, Endocarditis, Cardiac tumours like atrial myxoma
2)Non inflammatory Non atherosclerotic causes:
Arterial dissection, Marfans, Radition vasculopathy, Migraine, Fibromuscular dysplasia, CADASIL.
3) Inflammatory:
Takayasu arteritis, Giant cell arteritis, Kawasaki disease, PAN, churg strauss, wegner, microscopic Polyangitis.
4) Infections: HIV , Tuberculosis, Hepatitis B, syphilis
5)Hypercoagulable states: Protein C , protein S and anti thrombon ||| deficiency, APLA , hyperhomocyteinemia, factor v leiden mutation, Sickle cell.
Approach to stroke in young:
| Clinical clue | Suspicion |
|---|---|
| Fever | Infection Connective tissue disease Vasculitis |
| Lymphadenopathy | Lymphoma Infection |
| History of asthma | Churg Strauss syndrome |
| History of recent head trauma | Arterial dissection In situ arterial thrombosis |
| Headache | Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) Arterial dissection Vasculitis Systemic lupus erythematosum (SLE) |
| Oral/genital ulcers | Syphilis SLE Behçet disease Herpes simplex |
| Butterfly erythema | SLE |
| Splinter hemorrhages underneath the nail | Endocarditis |
| Needle puncture signs | Drug use |
| Tattoos | HIV infection Hepatitis |
| Alopecia | Systemic lupus erythematosus (SLE) Temporal arteritis Cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy (CARASIL) |
| Xanthelasma | Hyperlipidemia |
Investigations:
First line investigations:
CBC, Lft, Rft , ECG , CXR, peripheral smear, ESR, CRP, HIV serology CT , MRI scan 2decho
Second line investigations:
MR angiography, RA factor , serum homocysteine levels, protein C , protein S , Anca levels, factor V , Holter monitoring , D Dimer levels.
Treatment : Treatment depends on the etiology of stroke and once etiology is identified then treatment is individualised.
Antiplatelets are given.
Rehabilitation after stroke is a multidisciplinary approach with physiotherapist, occupational therapy and speech language therapist.
https://www.intechopen.com/chapters/72380
--------------------------------------------------------------------------
SHORT CASE 1:
A 22 year old male resident came with complaints of
Distension of abdomen and
facial puffiness since 2years
Moon face present
Pink striae noted over anterior abdominal wall.
Thin skin present .
Buffalo hump present .
Skin examination - Multiple itchy erythematous annular leisons noted over groin and inner thigh region.
CBP - HB - 14.0g/dl
TLC - 10,700
PLT - 3.69lakhs.
RBS - 94 mg/dl
CUE - ALBUMIN -trace
SUGARS - NIL .
PUS CELLS - 2-4
RBC - NIL .
LFT - TB -1.03
DB-0.21
ALBUMIN - 3.9
RFT - UREA - 23
SERUM CREATININE - 1
ELECTROLYTES - Na - 141 meq/L
K- 4 meq/L
CL-98 meq/L
USG ABDOMEN -Normal.
We took dermatologist opinion for tenia incognito where they advised
FUSIDIC ACID CREAM.
SALINE COMPRESS OVER LEISONS.
Plan to start anti fungals on next visit once dose of steroids is reduced .
OPTHAL opinion Was taken to look for visual acuity and cataract .
No features of lens opacities noted .
We advised pt to get fasting 8am serum cortisol levels and was planned to start on low dose steroids to avoid adrenal crisis.
Summary
Time line with events and serum cortisol trends
In the month of June : ACTH STIMULATION TEST WAS DONE .
BY INJECTING 0.4 ML OF ACTOM PROLONGATUM INJECTION (ACTH) INTRA MUSCULAR @ 7am
1 HR LATER FASTING SERUM CORTISOL SAMPLE WAS SENT .
VALUE - 0. 35mcg/dl
Indicating there was HPA AXIS suppression and pt was started on TAB HIZONE 20mg per day in three divided doses @ 8am ,12 pm and 4 pm.
Pt was asked for follow up.
Systemic Side Effects of Topical Corticosteroids
Sandipan Dhar, Joly Seth, and Deepak Parikh
--------------------------------------------------------------------------------------------------
SHORT CASE 2 :
Concieved in the month of ? May 2016
Bleeding PV after two months of pregnancy for which she had been to hospital and was told about abortion for which Dilatation and curratage was done.
2017: september she concieved again and her 1 st and 2 nd trimester were uneventfull.
Edd was in the month of june 2018
She had been to doctor on 1st of june and usg turned out to be normal
Then she had been to doctor again on june 11 th as she had tightening of abdomen for which USG was done and was told as IUD as there was no fetal heart rate.
And then normal vaginal delivery was for bringing out iud .
2019 : February they had been to doctor in view of not concieving for which she underwent investigations and her
PLBS ? 210 and was started on OHA.
She was on OHA for 1 month.
2020May : LMP : 17/5/2021 she concieved for 3 rd time
And was again on OHA ( for 20 days)in the month of july and from august she was on
And when she had been on 24 th january to doctor as there was abdominal distension causing difficulty in sleeping and moving so she underwent usg showing polyhydromnios.
And she was operted ( Cesaerean section) at 7:00 pm ivo fetal bradycardia.
Baby cried immediatly after birth
Baby weight (boy) : 3200 grams.
And she was discharged on 28th january 2021
Her sugars were normal so after delivery she was not on any hypoglycemic agents.
Personal history:
General examination :
Patient moderately built and nourished
Height : 160cm
Weight :50kgs
GCS - E4 V5 M6
VITALS -
Pulse - 82 beats per minute, regular normal volume ,and character, no radio radial or radio femoral delay.
Blood pressure - 100/70 mm Hg, left arm supine position.
Respiratory rate - 18 cpm, thoracoabdominal.
Spo2- 98 % on room air
Jvp - not elevated.
Physical examination-
No pallor
No Icterus
No cyanosis
No clubbing
No generalized lymphadenopathy
No Pedal edema
Inspection -
Oral cavity - No dental caries and no Tobacco staining,no oral ulcers,chelosis or stomatitis
Abdomen - flanks full, distension.no visible scars or sinuses
No Umbilical hernia.
No Distended veins
No visible peristalsis or no visible pulsations.
Palpation -
Done in supine position with Both Limbs flexed and hands by side of body.
No tenderness or local rise of temperature.
Abdomen - soft, distended
No gaurding and rigidity
Lower border of liver palpable.
Spleen not palpable
Fluid thrill - present
Percussion -
Liver span - upper border of liver dullness in 5 th intercoastal space in mid clavicular line, lower border 3cm from coastal margin.
Auscultation :
Normal bowel sounds heard.
No hepatic bruit , venous hum or friction rub.
CVS : S1 S2 heard no murmurs
RS: BAE+ normal vesicular breatg sounds heard
CNS : No focal neurological deficit.
Provisional diagnosis:
Ascites secondary to exudative etiology ? Tuberculosis
Diabetes mellitus
Invetigations:
Hemogram: hb-9.6,
tlc-6700,
plt-4.38
Ascitic fluid amylase - 15
Ascitic fluid protein- 4.1and Sugar- 147
Ascitic fluid LDH- 431
Serology - HIV Hbsag Negative
LFT- TB-0.82,
Fbs-166
Plbs - 215
Sr.albumin-2.2
Ascitic albumin-1.7
Saag-0.5
Rft-
Cue-color-reddish
Alb-2+, sugars - nil, pus-10-12,epi cells-3-4, RBC-5-6,others- budding yeast cells present
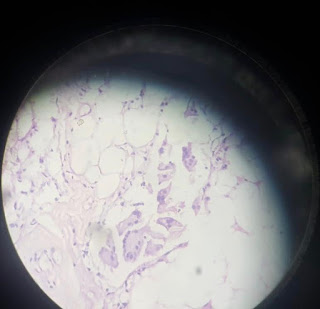
sections studied shows lobules of mature adipocytes with area showing chronic inflammatory cell infiltrate comprising of lymphocytes, epithelioid cells and plasma cells. occasional neutrophilic infiltrate seen. Fewvmultinucleated gaint cells seen.
Treatment :
1) Tab Isoniazid Rifampicin Pyrazinamide and Ethambutol fixed dose combinations 2 tablets a day
2) Tab Pyridoxine 40 mg OD
3) Tab Wysolone 40 mg OD and tapered over 8 weeks
4) Tab Pantop 40 mg OD
Pedagogy topic :
Multiple Myeloma
Evidence based Medicine and Critical appraisal :
Objective :
To investigate whether endovascular thrombectomy alone is non inferior to intravenous alteplase followed by endovascular thrombectomy for achieving functional independence at 90 days among patients with large vessel occlusion stroke.
Design :
Multicenter, randomized, noninferiority trial conducted at 33 stroke centers in China. Enrollment took place from May 20, 2018, to May 2, 2020. Patients were enrolled and followed up for 90 days (final follow-up was July 22, 2020).
Patients:
Patients (n = 234) were 18 years or older with proximal anterior circulation intracranial occlusion strokes within 4.5 hours from symptoms onset and eligible for intravenous thrombolysis.
Intervention:
Patients were randomized to the endovascular thrombectomy alone as one arm and other arm as combined intravenous thrombolysis with IV alteplase and endovascular thrombectomy.
Comparision:
The primary end point was the proportion of patients achieving functional independence at 90 days (defined as score 0-2 on the modified Rankin Scale; range, 0 [no symptoms] to 6 [death].
Result:
63 out of 116 patients in Endovascular thrombectomy group and 55 out of 118 patients in combined intravenous thrombolysis and Endovascular thrombectomy group achieved functional independence
















Comments
Post a Comment