20100006002 CASE PRESENTATION
LONG CASE
A 30-year-old male electrician by occupation from Nakrekal came to the hospital with chief complaints of weakness in the right upper limb and right lower limb since 15 months
Difficulty while speaking since 15 months
History of present illness:
Patient was a 30 year old electrician who used to climb up the cell towers for repair works
Born in the middle order with one elder brother & one younger brother
His daily routine include waking up at 7-8 am and going to work at 9am after having breakfast and returning home at 6-7 pm after a tiring work for 7-8 hrs
Married at the age of 25 yrs and has 2 children and used to live happily with his family & friends
But 15 months back his whole life was turned upside down when he developed sudden onset weakness in right upper limb & lower limb with mouth deviation to left side due to which he was not able to do his daily work of living & earning and he became dependant on family members
Patient was apparently asymptomatic 15 months back and then he developed weakness in the right upper limb and right lower limb which was sudden in onset and associated with on and off difficulty in speech.
Weakness was predominantly on the right arm than the right leg.
History of difficulty in speaking since 15 months - patient describes it as not able to tell what he wants to tell but able to write it down (word-finding pauses)
History of difficulty in buttoning the shirt, mixing the food, and writing present
History of slippage of footwear present
No difficulty in squatting and getting up from the squatting position, climbing stairs up and down
There was no diurnal variation of weakness
No difficulty in lifting the head off the pillow
No difficulty in rolling over the bed, getting up from the bed
No difficulty in breathing
No history of pain or muscle cramps or fasciculations and any involuntary movements
Able to feel clothes, feeling hot and cold water while bathing
No history of tingling, numbness, pricking-like sensation, band like sensation or sensation of walking on cotton wool
No history of neck pain, or back pain
No history of unsteadiness on closing his eyes and is able to walk in the dark
No history of loss of consciousness or alteration in sensorium or any bowel bladder involvement.
No history of Delusions/ Hallucinations/emotional disturbances
No history of alteration of smell, blurring of vision, diplopia, difficulty in chewing, hearing difficulties or dysphagia.
No history of giddiness, syncope, sweating, or palpitations
No history of bowel or bladder incontinence
No history of fever, headache, vomiting, or neck stiffness.
No history of calf pain, trauma, fall from height, or any drug intake.
Past history:
No history of similar complaints in the past.
No comorbid illness like Diabetes Mellitus, Hypertension, coronary artery disease, thyroid disease, HIV, Tuberculosis, malignancy, or surgeries.
Personal history:
Married And non-vegetarian with normal sleep and appetite.
No alcohol and smoking habits.
Regular bowel & bladder habits
Family history:
Nonconsanguinous marriage, With no similar complaints in the family.
No significant past treatment history.
Summary:
Onset: Acute
Progression: rapidly progressive
Neurological: Right hemiparesis with UMN-type facial Nerve involvement
Anatomical: cortex > subcortical
Etiology: secondary to vascular > inflammatory.
General examination:
Patient conscious, coherent, and oriented to time place person
Moderately built and nourished
No pallor, icterus, clubbing, koilonychia, lymphedema, and pedal edema.
Temperature: Afebrile
PR: 78 bpm, regular, normal in volume and character with no radio radial delay or radio femoral delay.
BP: 130/80 mm hg in the right and left arms.
RR: 16 CPM
Systemic examination:
Central nervous system:
Higher mental functions:
Level of Conscious Normal (GCS: 15/15)
Oriented to time place and person.
Speech and language :
spontaneous speech present
Comprehension present
Fluency absent
Repetition absent
Reading and writing present
Cranial Nerve Examination:
1st Cranial Nerve (Olfactory):
Sense of smell present
2nd Cranial Nerve (Optic):
Visual acuity, Field of vision, and color vision are present. Fundus is normal.
3rd,4th, and 6th cranial Nerves (Oculomotor, Trochlear, Abducens):
Extraocular movement And pupil size normal
Direct and indirect light reflexes present and accommodation reflex present
No ptosis and nystagmus
5th cranial Nerve (Trigeminal):
Sensations over the face present
Corneal conjunctival reflex present
7th Cranial Nerve (Facial):
Motor: Nasolabial fold absent on the right side
Orbicularis occuli and frontalis muscle normal
Tongue Sensations Normal
Corneal and conjunctival reflexes present
8th Cranial Nerve (Vestibulo-Cochlear):
Rinnes test and Weber test- No hearing loss.
9th and 10th cranial Nerve (Glossopharyngeal and Vagus):
Uvula and Palatal arch movements are normal and the gag reflex is present.
11th cranial Nerve (Spinal accessory):
Sternocleidomastoid and trapezius muscle normal
12th Cranial Nerve (Hypoglossal):
Tongue protrusion in the midline.
Gait: Hemiplegic circumduction gait
Motor System:
Bulk:
Inspection: Right thigh appears to be atrophied
Measurements:
Upper limb:
Right side 27.5 cms @ 10 cms above the olecranon & 24 cms @ 10 cms below the olecranon
Left side 29.5 cms @ 10 cms above the olecranon & 26 cms @ 10 cms below the olecranon
Lower limb:
Right side 46 cms @ 18 cms above the superior border of patella & 33 cms @ 10 cms below the tibial tuberosity
Left side 50 cms @ 18 cms above the superior border of patella & 33 cms @ 10 cms below the tibial tuberosity
Right. Left
Tone:
Upper limb. Normal Normal
Lower limb. Normal Normal
Power:
Upper limb:
Proximal muscles 4/5 5/5
Deltoid
Supraspinatus
Infraspinatus
Biceps
Triceps
Brachioradialis
Pectoralis and latismus
Dorsi muscle
Rhomboidus
Distal muscles. 0/5 5/5
ECR
ECU
Extensor digitorum
FCR
FCU
Lower limb:
Proximal muscles 4/5 5/5
Iliopsoas
Adductor femoris
Gluteus maximus
Gluteus medius and
minimus
Hamstrings
Quadriceps femoris
Distal muscles. 0/5 5/5
Tibialis anterior
Tibialis posterior
EDL
FDL
EHL
EDB
Reflexes: Right Left
Superficial reflexes
Corneal reflex. Present. Present
Conjunctival reflex. Present. Present
Abdominal reflex. Present Present
Plantar reflex. Extensor. Flexor
Deep tendon reflexes
Biceps. +++. +
Triceps. +++. +
Supinator. +++ +
Knee. +++. +
Ankle. +++ +
BICEPS
TRICEPS
Sensory system:
Spinothalamic tract: touch, pain, and temperature sensations are normal
Posterior column: vibration, position, and fine touch normal.
Cortical sensations: Graphaesthesias and stereognosis absent.
No cerebellar signs.
Cardiovascular system:
S1, S2 heard
No murmurs
Respiratory system:
Bilateral air entry and Normal vesicular breath sounds were heard.
Per abdomen:
Soft and no organomegaly.
Provisional diagnosis:
Cerebrovascular accident: Right-sided hemiparesis with Right UMN type of facial Palsy with Broca's aphasia secondary to left MCA territory involvement
Investigations:
Hemogram:
Hb: 15.7 gm/dl
TLC: 8,800 cells/cumm.
Platelets: 3.1 lakhs/cumm
RBS: 103mg/dl
LFT:
Total bilirubin: 0.64 mg/dl
Direct bilirubin : 0.18mg/dl
Total proteins:6.9
Albumin: 4.39
RFT:
Serum creatinine: 1.0 mg/dl
Blood urea:18mg/dl
Serum electrolytes: Normal
Fasting lipid profile: Normal
ESR: 20mm/hr
CRP: negative
APTT:34 sec
Bleeding time:2 min 30sec
Clotting time:4 min 30sec
D Dimer: 300 ug
RA factor: negative
CUE:
Albumin: Trace
Sugar: Nil
Pus cells:2-3cells/HPF
Epithelial cells:2-3cells/HPF
HIV: Non-Reactive
HbsAg: Non-reactive
VDRL: Negative
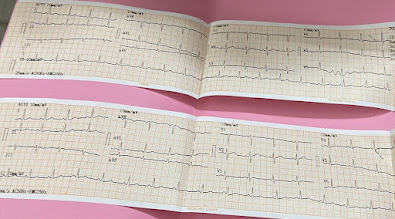
ECG:
12 lead ECG at 25 mm/sec showing sinus rhythm with regular RR interval with normal p wave QRS complex and T wave morphology
2d ECHO:
Normal LV systolic function
No regional wall motion abnormalities
EF: 62%
Chest x-ray :
Cxray PA views the inspiratory and non-rotated film.
Domes of the Diaphragm are clearly seen and well defined with no cardiomegaly
The right heart border and left heart border are clear with no Hilar lymphadenopathy or any Lymph node enlargement.
Bones and ribs appear normal.
MRI brain :
Final diagnosis:
Cerebrovascular accident: Right-sided hemiparesis with Right UMN type of facial Palsy with Broca's aphasia secondary to ischemic stroke involving left insula, temporal and front parietal regions (left MCA territory)
Treatment:
Physiotherapy of the right upper limb and lower limb.
Discussion:
Ischaemic stroke in young:
Definition:
Many authors consider the age of 45 years as the upper limit for stroke in young.
Epidemiology:
About 10-15% of strokes occur in younger patients, constituting approximately 2 million adolescents and young adults worldwide who suffer from an ischaemic stroke.
Risk factors:
Conventional risk factors like Diabetes Mellitus, Hypertension, and dyslipidemia.
Risk factors for stroke in young include smoking, alcohol, and drug abuse: cocaine IV drug users, and oral contraceptive pills.
Migraine with aura, Malignancy
Etiology:
1) Cardiac causes:
30% of stroke in young is secondary to cardiac causes: Congenital heart disease, PFO,
Atrial fibrillation, Acute MI, cardiomyopathy, Endocarditis, Cardiac tumors like atrial myxoma
2) Noninflammatory Nonatherosclerotic causes:
Arterial dissection, Marfans, Radition vasculopathy, Migraine, Fibromuscular dysplasia, CADASIL.
3) Inflammatory:
Takayasu arteritis, Giant cell arteritis, Kawasaki disease, PAN, Churg Strauss, Wegner, microscopic Polyangiitis.
4) Infections:
HIV, Tuberculosis, Hepatitis B, syphilis
5) Hypercoagulable states:
Protein C, protein S and antithrombin III deficiency, APLA, hyperhomocysteinemia, factor v leiden mutation, Sickle cell.
Approach to stroke in young:
|
CLINICAL CLUE |
SUSPICION |
|
Fever |
Infection |
|
Lymphadenopathy |
Lymphoma |
|
History of asthma |
Churg Strauss syndrome |
|
History of recent head trauma |
Arterial dissection |
|
Headache |
Cerebral autosomal dominant arteriopathy with subcortical
infarcts and leukoencephalopathy |
|
Oral/genital ulcers |
Syphilis |
|
Butterfly erythema |
SLE |
|
Splinter hemorrhages underneath the nail |
Endocarditis
|
|
Needle puncture signs |
Drug use |
|
Tattoos |
HIV infection |
|
Alopecia |
Systemic lupus erythematosus (SLE) |
|
Xanthelasma |
Hyperlipidemia |
Investigations:
First-line investigations:
CBC, Lft, Rft, ECG, CXR, peripheral smear, ESR, CRP, HIV serology CT, MRI scan 2decho
Second-line investigations:
MR angiography, RA factor, serum homocysteine levels, protein C, protein S, Anca levels, factor V, Holter monitoring, D Dimer levels.
Treatment:
Treatment depends on the etiology of the stroke and once etiology is identified then treatment is individualized.
Antiplatelets are given.
Rehabilitation after stroke is a multidisciplinary approach with physiotherapists, occupational therapists, and speech-language therapists
---------------------------------------------------------------------------------------------------------------
SHORT CASE I
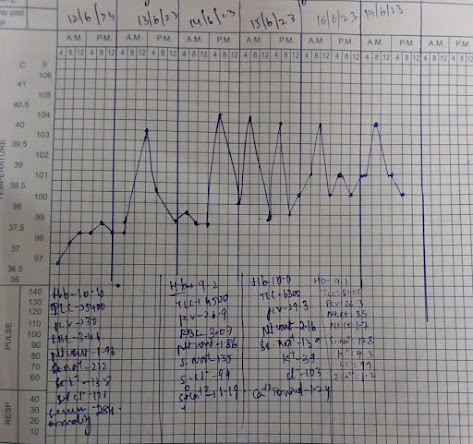
A 50 years old male, mason by occupation and resident of Bhongir, came to the hospital with chief complaints of fever since 2 months, and loss of appetite since 2 months.
History of presenting illness
A 50-year-old mason who was happily living with his family daily wakes up at 5 am, goes for a walk to get milk, and returns home. He then has tea with biscuits and rice for breakfast, then leaves for his work by 9 am. He has rice, for lunch, with curries at his workplace. He comes back from work at either 7 or 8 pm. He has rice for dinner at 9 pm and goes to sleep by 10 pm.
2 months back while he was working he felt generalized weakness & body pains for which he left work early and went to home. The next day morning he had fever for which he bought some tablets from a local pharmacy.
2 days later he was taken to a local ayurvedic by his family members on suspicion of jaundice where he was given some herbal medicine 3 doses (1 dose/week) and advised of some dietary restrictions.
Even after 3 weeks, his fever doesn't come down and he felt no change in his general condition.
He also lost his appetite gradually since 2 months, and history of weight loss since 2 months.
Since 20 days, his fever increased usually more in the evenings which would continue the whole night, and reduce by morning, and is associated with chills for which he was brought to our hospital.
Patient also complained of on & off pain in the abdomen in the umbilical and right lumbar region, which was insidious in onset, gradually progressive, non-radiating, aggravated while walking (around 100 meters), and relieved on rest.
H/o burning micturition present
No h/o urgency, frequency, incontinence, polyuria, polydipsia, nocturia, or urethral discharge.
No h/o sore throat, cough, or cold
No h/o vomiting, diarrhea
No h/o rash over the body, bleeding gums, Malena
No h/o headache, photophobia, involuntary movements, altered behavior
No H/o pedal edema, SOB, chest palpitations, chest pain, and tightness.
Past History
Patient is a known case of pulmonary tuberculosis 25 years ago, for which he used ATT for 6 months.
Not a known case of DM, HTN, CVA, CAD, thyroid disorders, asthma, and epilepsy.
Personal history
Diet - mixed
Appetite - decreased since 2 month
Bowel & Bladder habits: Regular
Sleep - decreased
Addictions - 90 ml occasionally since 35 years.
Family history
No similar complaints
Surgical history
Appendicectomy was done 30 years ago
General examination
Examination was done in a well-lighted room, with consent and informing the patient in the presence of a female attendant.
Patient was conscious, coherent, and cooperative, well oriented to time, place, and person.
Pallor - present
Icterus- absent
Cyanosis- absent
Clubbing - absent
Lymphadenopathy- absent
Pedal edema - absent
Vitals
Temperature- 38⁰ C
PR - 105bpm
RR - 23 CPM
BP - 100/60 mmHg
SpO2 - 99% at RA
GRBS - 114mg/dl
SYSTEMIC EXAMINATION
RESPIRATORY SYSTEM
Patient examined in the sitting position
Inspection
Lips and tongue normal
Oral candida - absent
Poor oral hygiene
Trachea appears to be central
Shape appears to be elliptical, B/L symmetrical
Mild wasting seen on right side supra scapular & infrascapular region
Respiratory movements appear equal on both sides and abdominothoracic type
No scars, sinuses, and dilated veins.
No lumps and Lesions
No intercostal recession
Palpation
All inspectory findings are confirmed
Apical impulse felt at 5th intercostal space and at the midclavicular line
Total circumference - 34 inches
Hemithorax, Right - 17 inches Left - 17 inches
Anterior Posterior - 8 inches
Transverse - 12 inches
Chest expansion - 2 cms
Tactile vocal fremitus - Right Left
Supraclavicular -. increased normal
Infraclavicular- increased. normal
Mammary- increased normal
Axillary- normal normal
Infra axillary- normal normal
Suprascapular- normal normal
Interscapular- normal normal
Infrascapular- normal normal
Percussion
Resonant in all regions
Auscultation
Fine crepitations were heard in the infraclavicular area.
Normal vesicular breath sounds in other areas.
Vocal Resonance - Right Left
Supraclavicular - increased normal
Infraclavicular- increased normal
Mammary- increased normal
Axillary- normal normal
Infra axillary- normal normal
Suprascapular- normal normal
Interscapular- normal normal
Infrascapular- normal normal
ABDOMINAL EXAMINATION
Inspection
Shape - scaphoid
Umbilicus- centralized, inverted
Scar present of appendicectomy
No dilated veins
No visible pulsations or peristalsis
Palpation:
Soft, tenderness present in epigastrium & hypogastrium
Deep palpation-
No organomegaly
Percussion:
No fluid thrill
Liver span 12 cms
Auscultation:
No bowel sounds heard
CVS EXAMINATION
Inspection:
Shape of the chest- elliptical
No engorged veins, scars, visible pulsations
Palpation:
Apex beat can be palpable in the 5th intercostal space
Auscultation:
S1,S2 are heard
No murmurs
CNS EXAMINATION
Higher mental functions: intact
Cranial nerves intact
Motor examination: R L
Bulk. N N
Tone. N N
Power. N N
Reflexes:
Biceps. 2+ 2+
Triceps. 2+ 2+
Supinator 2+. 2+
Knee 2+.2+.
Ankle. 2+. 2+
Sensory examination: Normal
No meningeal signs
Investigations
Hemogram:
Hb - 10g/dl
PCV -29.3 vol%
Total leucocyte count - 6,300cells/cumm
RBC -3.08millions/cumm
Platelets-2.16lakhs/cumm
Serum electrolytes:
Sodium-134mEq/l
Potassium-3.9mEq/l
Chloride-103mEq/l
RFT:
Creatinine-1.2mg/dl
Urea -41mg/dl
LFT:
Total bilirubin-1.26mg/dl
Direct bilirubin-0.30mg/dl
AST-88IU/L
ALT-72IU/L
ALP-140IU/L
Total proteins-8.3gm/dl
Albumin-2.95gm/dl
RBS-94mg/dl
Serology:
HIV - Reactive
Anti-HCV antibodies -Nonreactive
HbsAg- Non reactive.
USG Abdomen:
Diagnosis:
Denovo Detected RVD + with ? Pulmonary TB reactivation
L2 wedge compression Fracture ? Osteoporotic / Pott's spine
Right upper lobe fibrosis with traction bronchiectasis - old TB sequelae
K/c/o Pulmonary TB 25 yrs ago
----------------------------------------------------------------------------------------------------------------
SHORT CASE II
A 55-year-old male, resident of Nalgonda, who is a farmer by occupation came to the hospital with chief complaints of breathlessness since 6 months
• HOPI :
Patient was apparently asymptomatic for 20 years then had muscle cramps, increased frequency of urination, and giddiness for which he went to hospital and was diagnosed with DM type II and is on medication (T.Glymiperide + Metformin) since then.
1 year back he had generalized weakness, polydipsia, polyurea, and dizziness, visited the hospital and was found to have uncontrolled DM 2 and is on insulin ( since then.
Until 6 months ago he worked as a farmer, waking up at 5 am. he takes his breakfast at 7 am. Then he goes to work, has lunch at 1 pm. returns to home at 6-7 pm & has dinner at 8 pm, and goes to bed at 9 pm.
But 6 months back his whole life was changed when he was taken to the hospital after experiencing palpitations, dizziness, blurring of vision, and involuntary movements involving his upper limbs & body, where he was diagnosed with hypertension & Renal failure.
H/o SOB since 6 months NYHA 1-2 and from last 1-month shortness of breath increased NYHA 3-4, gradually progressive, associated with orthopnea & PND for which he came to our hospital.
H/o Low backache since 1 month
H/o itching all over the body with darkening of skin since 1 month
H/o decreased Urine output since 1 month
No thin stream, poor flow, increased frequency, hesitancy, or Burning micturition present.
No h/o Fever, Chest pain, Palpitations, Syncope
No h/o Cough
No other complaints
•Past History :
K/c/o DM-type II since 20 years
K/c/o hypertension since 6 months
No history of asthma, TB, epilepsy, thyroid abnormalities
•PERSONAL HISTORY:
Diet: Mixed
Appetite: Normal
Sleep: Disturbed
Bowel: Regular
Bladder: Decreased urination.
Habits: Do not consume any form of alcohol or tobacco.
●FAMILY HISTORY:
Not significant
●DRUG HISTORY:
HAI & NPH 3 units (three times a day) Insulin for the past 1 year,
TELMA for hypertension since the past 6 months
●GENERAL EXAMINATION:
The patient was examined in a well-lit room after obtaining consent.
The patient was conscious, coherent, and cooperative. He was moderately built and moderately nourished.
Pallor: Absent
Icterus: Absent
Cyanosis: Absent
Clubbing: Absent
Generalized Lymphadenopathy: Absent
Pedal Edema: Absent
Vitals :
Temperature - Afebrile
BP - 130/80 mm Hg
Pulse - 78 BPM
RR - 24 CPM
Rbs - 124 mg/dl @ 7pm
●SYSTEMIC EXAMINATION:
Cardiovascular system:
•Inspection:
Shape of the chest appears to be elliptical & bilaterally symmetrical
Apex beat is not visible
No scars, sinuses, dilated veins
No precordial bulge is seen.
•Palpation:
All inspectory findings are confirmed
Trachea is central
Apex beat felt at 6th intercostal space 1cm lateral to midclavicular line.
•Auscultation:
In Aortic, Pulmonary, Tricuspid & Mitral areas
S1 and S2 heard.
No murmurs heard
Respiratory system:
•Inspection
Shape of chest appears to be elliptical and bilaterally symmetrical.
Trachea appears to be central
No scars, sinuses, or engorged veins.
Symmetrical expansion of the chest
•Palpation:
All inspectory findings are confirmed
Trachea appears to be central
Tactile vocal fremitus normal in all areas
•Percussion:
Resonant note is heard in all areas
•Auscultation :
Normal vesicular breath sounds are heard.
No adventitious breath sounds.
ABDOMEN:
obese abdomen
Moves symmetrically with respiration
Umbilicus is central and inverted
No scars or sinuses
No local rise in temperature
No organomegaly
CNS:
Higher mental functions intact.
Motor examination:
Power: B/l Upper limbs: 4 + bilaterally
B/l Lower limbs: 4 + bilaterally.
Tone: Normal
Reflexes: R L
Biceps: 2+ 2+
Triceps: 2+ 2+
Knee: 2+ 2+
Ankle: 2+ 2+
Sensory examination: normal.
Cerebellar examination: normal.
Cranial nerve examination: normal.
Provisional diagnosis:
Acute on chronic LVF
Chronic renal failure since 6 months with?Uremic pruritis
●Investigations :
X-Ray chest
Interpretation :
Cardiomegaly
• Treatment :
Fluid restriction <2L /day
Salt restriction <2g /day
INJ HAI & NPH 3Units
Tab Lasix 40 mg BD.
Tab Nicardia 20 mg PO/TID
Tab Arkmain 0.1mg PO/TID
Tab Orofer -XT PO/OD
Hemodialysis.









































Comments
Post a Comment