20100006005 CASE PRESENTATION
LONG CASE .
21 year old woman, working as a nurse in an outside hospital, residing at Nalgonda presented to casualty on 26/8/2021 with the chief complaints of
CRANIAL NERVE | TEST | RIGHT | LEFT |
I | Sense of smell i) Coffee |
+ |
+ |
II | i) Visual acuity – Snellen Chart ii) Colour vision – Ishihara chart iii) Fundus | 6/6 Normal Normal | 6/6 Normal Normal |
III, IV, VI | i) Extra-ocular movements ii) Pupil – Size iii) Direct Light Reflex iv) Consensual Light Reflex v) Accommodation Reflex vi) Ptosis vii) Nystagmus viii) Horners syndrome | full 3mm Present Present Present Absent Absent No | full 3mm Present Present
Absent Absent No |
V | i) Sensory -over face and buccal mucosa ii) Motor – masseter, temporalis, pterygoids iii) Reflex a. Corneal Reflex b. Conjunctival Reflex c. Jaw jerk | Normal Normal
Present Present Present | Normal Normal
Present Present Present |
VII | i) Motor – nasolabial fold occipitofrontalis orbicularis oculi orbicularis oris buccinator platysma ii) Sensory – Taste of anterior 2/3rds of tongue(salt/sweet) Sensation over tragus iii) Reflex – Corneal Conjunctival iv) Secretomotor – Moistness of the eyes/tongue and buccal mucosa |
Present Good Good Good Good Good
Normal
Normal
Present Present
Normal |
Present Good Good Good Good Good
Normal
Normal
Present Present
Normal |
VIII | i) Rinnes Test ii) Webers Test
iii) Nystagmus | Positive Not lateralised
Absent | Positive
Absent |
IX, X | i) Uvula, Palatal arches, and movements
ii) Gag reflex iii) Palatal reflex | Centrally placed and symmetrical
Present Present |
Present Present |
X1 | i) trapezius ii) sternocleidomastoid | Good Good | Good Good |
XII | i) Tone ii) Wasting iii) Fibrillation iv) Tongue Protrusion to the midline and either side | Normal No No Normal | Normal No No Normal |
Bulk - Right Left |
III – POWER a. Neck muscles b. Upper limbs i) Shoulder Flexion-Extension Lateral Rotation-Medial Rotation Abduction -Adduction ii) Elbow Flexion-Extension iii) Wrist Dorsi flexion-Palmar flexion Abduction-Adduction Pronation-Supination iv) small muscles of hand v) Hand grip
c. Lower limbs i) Hip Flexion-Extension Abduction-Adduction Lateral Rotation-Medial Rotation ii) Knee Flexion-Extension iii) Ankle Dorsi flexion-Plantar flexion Inversion-Eversion iv) Small muscles of foot
d. Trunk muscles e. Beevor’s sign
|
Good
4+/5 4+/5 4+/5 4+/5 4+/5 4+/5 4+/5 4+/5 Good Good
2/5 2/5 2/5
2/5
2/5 2/5 2/5 Weak
|
Good
4+/5 4+/5 4+/5 4+/5 4+/5 4+/5 4+/5 4+/5 Good Good
2/5 2/5 2/5
2/5 2/5 2/5 2/5 Weak |
TEST | RIGHT | LEFT |
I – SPINOTHALAMIC 1. Crude touch 2. Pain 3. Temperature II – POSTERIOR COLUMN 1. Fine touch 2. Vibration 3. Position sense 4. Romberg’s sign III – CORTICAL 1. Two point discrimination 2. Tactile localisation 3. Graphaesthesia 4. Stereognosis |
Reduced Reduced Reduced
Reduced Reduced Lost Unable to perform
Lost Lost Lost Normal |
Reduced Reduced Reduced
Reduced Reduced Lost Unable to perform
Lost Lost Lost Normal |


USG ABDOMEN - No sonological abnormality detected
---------------------------------------------------------------------------------------------------------------------------------------
SHORT CASE I
A 50 year old Male came with chief complaints of abdominal distension since 4 days associated with shortness of breath since 3 days.
H/0 of yellowish discoloration of eyes 2 months back subsided, now started again since 4days
No h/0 of nausea and vomitings,
No h/0 of pain abdomen
No h/0 of decreased urine output
No h/0 of high coloured urine and clay coloured stools.
No history of blood transfusions
No bleeding manifestations.
No H/o usage of TB drugs or any other medication.
Pedal edema- Present (pitting type)
HEAD TO TOE examination:
Axillary hair loss seen
No parotid swelling
Palmar erythema absent
Hyperpigmented patches seen on palm
Gynaecomastia present but non tender
Pale colour nails absent
Tremors absent
Spider naevi not seen
Petechiae, purpura not seen
GENERAL EXAMINATION
Patient is conscious, Oriented, Comfortable, Co-operative
afebrile
Pallor - present
Icterus - present
Cyanosis – negative
Clubbing – no
Pedal edema – bilateral, painless, pitting
No Significant lymphadenopathy
TROISIER’S SIGN - Negative
EXTERNAL MARKERS OF LIVER CELL FAILURE -
HEAD AND NECK– No alopecia, no bitots spots, no xanthelasma , subconjunctival hemorrhage, pallor +, icterus+, no medial supraciliary madarosis, sunken eyes and cheeks, loss of facial hair, no parotid enlargement, bleeding gums
TRUNK – no spider nevi, no gynaecomastia, loss of pectoral/axillary hair present , no dilated veins, wasting, abdominal distension present , no caput medusae, no loss of pubic hair, no testicular atrophy, no scratch marks, purpura
UPPER LIMBS – left side dupuytrens contracture present , no bounding pulse, no clubbing, no flapping tremor, no palmar erythema, no pruritic marks
LOWER LIMBS – Pedal Edema present
NO BONY TENDERNESS, GUM HYPERTROPHY, LEUKEMIA CUTIS
VITAL SIGNS
PULSE: 82 bpm regular rhythm,normal volume, felt in all peripheral pulses,no radioradial/radiofemoral delay,no apex pulse deficit
BLOOD PRESSURE: 110/80 mm of Hg measured in the left Upper limb with the patient in sitting position
RESPIRATORY RATE: 16/min, regular abdominothoracic
TEMPERATURE: 98.2 F measured in the Axilla
SYSTEMIC EXAMINATION
EXAMINATION OF THE ORAL CAVITY- normal
ABDOMEN:
INSPECTION:
1. Shape – distended
2. Flanks –full
3. Umbilicus –everted, no nodules
4. Skin – no stretched, shiny, scars, sinuses, striae, nodules, scratch marks, puncture marks
5. No Dilated veins – front/back
6. Movements of the abdominal wall equal in all quadrants with respiration,
no visible gastric peristalsis,
7. Normal Hernial Orifices, no cough impulse
8. External genitalia - Normal
PALPATION:
Superficial Palpation – Tenderness, Warmth, Direction of Blood Flow in Veins
Deep Palpation
1. Liver : non-tender,
non-pulsatile
Right hypochondrium about 1 cms below the Right costal margin in the Mid clavicular line
Which moves with respiration and is
firm in consistency with a irregular surface
And a rounded edge
And I am not able to make out the upper border on Palpation
Probably an Enlarged liver
2. Spleen
no significant spleenomegaly
Palpation by Dipping in the case of Tense Ascites
Measurements - Abdominal Girth
Spino-Umbilical Distance
Distance between the Xiphisternum-Umbilicus and Umbilicus-Pubic Symphysis
External Genitalia - normal
PERCUSSION:
1. Shifting dullness - present
2. Percussion of Liver for Liver Span - Noat able to palpate
3. Tidal Percussion
AUSCULTATION:
1. Bowel sounds present – 10 to 15/min for small bowel, 3 to 5/min for large bowel
2. Bruit not heard
3. No Venous Hum
PER RECTAL EXAMINATION: stool stained
EXAMINATION OF OTHER SYSTEMS
CARDIOVASCULAR SYSTEM:
S1, S2, no murmurs heard.
EXAMINATION OF RESPIRATORY SYSTEM:
No Added sounds
EXAMINATION OF NERVOUS SYSTEM:
no Flapping tremor, Peripheral Neuropathy
DIAGNOSIS
CHRONIC DECOMPENSATED LIVER DISEASE, CIRRHOSIS WITH PORTAL HYPERTENSION WITHOUT EVIDENCE OF HEPATIC ENCEPHALOPATHY
TREATMENT:
Fluid restriction
Salt restriction
1)TAB LASIX 40 mg/BD
2)TAB ALDACTONE 50 mg /BD
3)TAB UDILIV 300 mg po /BD
4)Syrup LACTULOSE 20 ml po /TID
-----------------------------------------------------------------------------------------------------
SHORT CASE II
This is a case of a 45 year old female,resident of Nalgonda, technician by occupation came to the op with the chief complaints of
1) C/O multiple joint pains and swellings since 15 years
2) c/o generalised weakness and easy fatiguability since 6 months
History Of Presenting Illness:
Patient was born out of non consanguionus marriage and had 2 siblings .
at 15 yrs of age - Got married in 10th class (Non consanguinous marriage) Her partner was a from rich family where he doesnt used to go to job and used to drink alchol through out the day . and used to come back to home by evening and started to physically and mentally abuse our patient.
AT 18 YEARS - She gave birth to a healthy first male child through LSCS(No significant medical history was given for indication of LSCS)
AT 20 YEARS- Gave birth to a healthy baby girl through LSCS
She used to be a homemaker initially.
Due to her husband’s aggressive behaviour, she ingested pesticide which was seen by her sister.
immediately She was given some saltwater (which was home remedy to induce vomiting),induced vomitings and later she was shifted to Osmania hospital where she was admitted for 2 days and treated for ?organophosphorous poisoning.
Later she came away from her husband with her children for their education and
20 YEARS BACK (JAN 2003)-She joined as a technician in our hospital and also worked as a tailor
17 YEARS BACK(in 2006)-
One fine day patient initially observed left ankle swelling and left leg edema which initially resolved overnight but later didn’t seem to resolve with rest.
3-4 months later , she c/o bilateral lower limb edema about which she neglected due to her work stress
Gradually over a period of time , She also c/o pain in the large joints (ankle, knee, wrist ,elbow ,shoulder) and also neck pain .
There was no h/o small joint involvement
She used homeopathy medication but the pain didn’t seem to resolve
7 YEARS BACK (2016)
Visited this hospital due to severe pain in the joints, and diagnosed to be having
anti CCP positive, ANA negative.
diagnosed with Rheumatoid arthritis and
She was started on Intraarticular triamcinolone and NSAIDs
During one of her routine checkups, she also c/o increase in her weight for which Thyroid profile is done and she was diagnosed with HYPOTHYROIDISM. She was kept on Tab. Thyronorm 25mcg PO/OD
5 YEARS BACK (2018)
She was also kept on Tab.Wysolone 5mg PO/OD(used it for 3 years) and Tab.Methotrexate (15mg) PO/OD
4 YEARS BACK(2017)
She was also kept on Hydrochloroquine (used it till 2022)
Also on Tab.Sulphasalazine 1000mg
2 YEARS BACK
Due to medication she c/o Recurrent epigastric pain and bloating like sensation where she underwent endoscopy and diagnosed with gastric ulceration since then patient is on PPI's.(Tab Rabeprazole 40mg once daily)
AUGUST 2022
During one of her routine investigations she was diagnosed to be having Type2 Diabetes Melkite’s for which she was kept on Tab.Metformin 500mg PO/OD
Past History
PERSONAL HISTORY
DIET- Mixed
APETITE- Good
BOWEL AND BLADDER MOVEMENTS -Regular
SLEEP -Adequate
ADDICTIONS -none
MENSTRUAL HISTORY -
Age of Menarche -13 yrs
Periods -regular 5/28
No of pads-3/ days
Pain and clots absent
FAMILY HISTORY - No significant family history noted .
Social & Educational History
Localisation of Chronic Problem
This 45 year old woman has a 15 year history of bilaterally symmetrical progressive inflammatory polyarthritis. Features favouring an inflammatory pathology are -
- Features of inflammation such as severe pain associated with edema of the joints and limitation of range of active movements
- Early morning stiffness, lasting for more than 30 mins (for 1 hour in this patient)
- Pain and edema of joints improving with activity and worsening with rest
- Features of uncontrolled systemic inflammation such as fever, involuntary loss of weight associated with loss of appetite.
- Swellings at joints and deformation of normal joint posture
Provisional Diagnosis - Bilaterally Symmetric Chronic Progressive Inflammatory erosive Peripheral Polyarthritis
Clinical Examination
Supine Position
Sitting Position
Head to Toe General Examination
Ht-155cm
Wt-74 kgs
- Palpation - no increase in temperature on both sides
Other Systems Examination
INVESTIGATIONS
CBP
Hb-9.8
TLC-8600
N/L/E/M/B-68/25/2/5/0
Platlets -4.5
MICROCYTIC HYPOCHROMIC ANAEMIA
FBS-106
PLBS-241
HbA1c-7.0
THYROID PROFILE
T3-1.06
T4-12.03
TSH-4.15
LIPID PROFILE
Total cholesterol-190
Triglycerides-238
HDL-39
LDL-118
VLDL-47.6
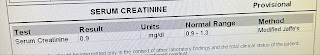
RFT
Urea-24
Creatinine -0.7
Uric acid-2.2
Calcium-9.3
Phosphorus -3.1
Sodium-135
Potassium-4.6
Chloride-101
LFT
Total bilirubin-0.60
Direct bilirubin -0-15
SGOT-22
SGPT-17
ALP-173
Total proteins-5.8
Albumin -3.5
A/G ratio-1.58
- Rheumatoid Arthritis (most likely)
- Rheumatoid Arthritis with coexistent Gout
- Psoriatic Arthritis
- Enteropathic Arthritis
- Reactive Arthritis
- SLE






























































Comments
Post a Comment