20100006006 CASE PRESENTATION
LONG CASE
Chief compliants:
1) Slowness of movements since 1 year .
2) Involuntary movements of the Left upper limb.
3) Slowness in speech since 1 year.
History of present illness:
60
year old female,who is a mother of 3 children ( 1 son and 2 daughters
), labour by occupation ( goes to agriculture field ) was apparently
asymptomatic 1 year back, then developed Slowness of movements which was
insidious onset, gradually progressive not associated with any weakness
associated with difficulty in initiation of movement and difficulty in
day to day activities .The difficulty was in such a way that she could
not even comb the hair, mix the food and bathing.
History
Involuntary movements of the left upper limb since 1 year , occuring at
rest ,aggravated by emotional stress and disappeared during sleep and
movement.
History of associated postural changes .
No History of sensory disturbances
No History of anosmia.
History of sleep disturbances- present
No History of Genito urinary and Gastro intestinal disturbances.
No History of Dysphagia
No History of fever , convulsions and coma
No History of head injury
No History of yellowish discoloration of eyes
No History of usage of any antipsychotic drugs.
Family History:
No Significant family History
Personal history:
Mixed diet
Normal bowel and bladder
Sleep:
Past history:
No history of similar complaints in the past .
No history of Diabetes, Hypertension, Cerebrovascular disease, Cardiovascular disease .
General Examination:
Patient is conscious and Co operative.
Facies :
Infrequent blink with Starring look.
Loss of facial expression.
No pallor, icterus, Cyanosis, clubbing,lymphadenopathy, edema
Pulse :
BP: supine - 110/70mmhg
PR: 80bpm
Standing - 100/70 mmhg.
PR: 90 bpm
Posture : stopped posture.
Neurological examination:
1. HIGHER MENTAL FUNCTIONS:
a. Consciousness- Normal
b. Orientation to time, place and person- present.
c. Speech and language -slow speech.
d. Memory -Normal
e. Delusions, hallucinations- No
f. Emotional lability
g. MMSE score
I. Orientation
1.date, day, mönth, season, year -4
2. floor, hospital. District, state, country- (5)
II. Registration
Name three objects taking one second for each obiect. Ask him to repeat the same
Repeat till he remembers (3)
III. Attention and Calculation
Serial 7's 5 times - 4 points.
IV. Recall
Recall the three objects (3)
V. Language
I. Name 2 obiects (2)
2. Repeat a sentence (1)
3. Follow a 3 stage command (3)
4. Reading "close your eyes"- Not done.
5. Writing a sentence - Cannot write.
6. Copy a design (1)
TOTAL SCORE- 26/30
2] CRANIAL NERVES.
I) Sense of smell - Normal on both sides.
II) On Right side - No perception of light
On left side - Visual acuity, colour vision - Normal.
III,IV,VI)
i) Extra-ocular movements - Normal in both eyes .
ii) Pupil - Size - 2-3 mm in both eyes.
ili) Direct Light Reflex - Sluggish in right eye
Constriction of pupil- left eye.
iv) Consensual Light Reflex- Absent in left eye.
v) Accommodation Reflex - Absent in right eye,
vi) Ptosis - absent vil) Nystagmus - absent
V)
i) Sensory -over face and buccal mucosa -presen
il) Motor - masseter, temporalis, pterygoids- normal
iii)
Reflex
a.Corneal Reflex - present in both eyes.
b. Conjunctival Reflex - present in both eyes. C.Jaw jerk - absent VII)
i) Motor - intact on both sides il) Sensory -
Taste of anterior 2/3rds of
tongue- present.
Sensation over tragus
iii) Reflex -
Corneal-
present
Conjunctival- present.
8)
i)
Rinnes Test - AC more than BC ii) Webers Test-
unable to perceive the vibrations when tuning fork - kept on fore head.
IX,X)
i) Uvula, Palatal arches, and movements- Normal
¡¡)Gag reflex - Present
iii) Palatal reflex- Present
XI)
i)
trapezius- able to perform .
¡¡)sternocleidomastoid -slight difficulty in turning
XII)
¡)Tone-Normal
¡¡)wasting- No
iii) Fibrillation-No iv) Movements - normal.
3] Motor system
I- BULK
a. Inspection - Normal
b. Palpation - Normal
c. Measurements
Upper limb- MAC -30 cm on both sides.
Lower limb-MLC - 31cm on both sides
II - TONE
a.Upper limbs- Fluctuant rigidity in upper limbs - Cog wheeling type .
b. Lower limbs- rigidity experienced throughout movement - Lead pipe type.
III - POWER
a. Neck muscles- 5/5
b. Upper limbs
i)Shoulder
Flexion-Extension-5/5
Lateral Rotation-Medial Rotation-5/5
Abduction -Adduction-5/5
ii)Elbow
Flexion-Extension-5/5
iii)Wrist
Dorsi flexion-Palmar flexion-5/5
Abduction-Adduction-5/5
Pronation-Supination-5/5
iv)small muscles of hand-5/5
V)Hand grip- Normal.
с.Lower limbs
i)Hip
Flexion-Extension-5/5
Abduction-Adduction-5/5
Lateral Rotation-Medial Rotation-5/5
ii)Knee
Flexion-Extension-5/5
iii)Ankle-
Dorsi flexion-Plantar flexion-5/5
Inversion-Eversion-5/5
IV -REFLEXES
A. SUPERFICIAL REFLEXES( Both sides )
1. Corneal- Present
2. Conjunctival- Present.
4. Palatal Reflex-present
5. Abdominal Reflex-present
5. Plantar Reflex- Negative.
B. DEEP TENDON REFLEXES( Both sides )
1. Jaw jerk- Absent
4. Biceps jerk- +2
5. Triceps jerk-+2
6. Supinator jerk-+2
7. Finger flexion reflex- no response.
8. Knee jerk-+2
9. Ankle jerk-+2
10. Clonus- Absent
VI GAIT- Video
VIl - INVOLUNTARY MOVEMENTS- Absent
A - Athetosis, Asterexis
B- Ballismus
C - Chorea
D- Dystonia
E - Essential tremors
F -Fasciculations
M - Myoclonus
4]SENSORY SYSTEM
TEST
I - SPINOTHALAMIC( Both sides )
1. Crude touch- Normal
2. Pain- Normal
3. Temperature- Normal
II - POSTERIOR COLUMN
1. Fine touch- Normal
2. Vibration- Normal
3. Proprioception - Normal
4. Romberg's sign- negative
III - CORTICAL( both sides )
1. Tactile localisation- present
2. Graphaesthesia- Present
3. Stereognosis- present
5]CEREBELLAR SIGNS
Coordination( on both sides )
a. Upper Limbs - Finger Nose test, Finger Finger Nose test, Drawing a circle,
Putting a dot in the centre of the circle ~ Present
b. Lower Limbs - Heel Knee test
c. Dysdiadokokinesia- Absent
6. AUTONOMIC NERVOUS SYSTEM
Postural Hypotension
Resting tachycardia
Abnormal sweating
7. SIGNS OF MENINGEAL IRRITATION
Neck stiffiness- Absent
Kemig's sign-Absent
Brudzinski's sign-Absent
Examination of other systems:
CARDIOVASCULAR SYSTEM:
JVP- Not raised ,Apex normally placed, no Palpable P2, Heart sounds - normal, No thrills/murmurs
RESPIRATORY SYSTEM:
Chest symmetrical, No paradoxical movements, Normal vesicular breath sounds heard,
No abnormal/added sound
ABDOMEN:
Abdomen is soft, No organomegaly, No ascites.
Test for extensor digitorum brevis
Tibialais posterior.
Ilio psoas
Interossei muscle testing
Adductor pollicis
Testing for pain:
DIAGNOSIS
INVESTIGATIONS:
RBS- 91mg/dl
Blood urea- 28mg/dl
Serum creatinine - 0.7mg/dl
CUE
Colour: pale yellow
Appearance: Clear
Albumin NIL
Sugar NIL
Bile salts and pigments NIL
Pus cells: 2-3
Epithelial cells: 2-3
RBC NIL
Crystals, casts NIL
Amorphous deposits NIL
HEMOGRAM
HB: 13.2
TLC: 7700
N/L/E/M: 53/33/4/10
PCV: 40.3
MCV: 82.3
MCB: 27.1
MCHC: 32.8
RBC: 4.87
PLT: 3.5
LFT
TB: 1
DB: 0.2
AST: 17
ALT: 9
ALP: 148
TP: 7.4
ALBUMIN: 4.0
A/G: 1.2
HIV- negative
HBsAg- negative
HCV- negative
ECG:
CXR- PA
TREATMENT:
1) Tab Syndopa ( levodopa 100mg+ Carbidopa 25 mg) PO/OD
----------------------------------------------------------------------------------------------------------------
SHORT CASE I
Chief complaints:
Multiple joint pains since 7 years.
History of present illness :
Patient
was a Taylor in the medical institute, her daily routine was to stitch
the clothes with the help of machine from 9am to 4 pm in the medical
institute.
She was apparently normal 7 years
back , then developed pain in the right proximal interphalangeal joints
association with stiffness in the early morning for about 1 hour and
which gradually relieved after 2 hours of getting from the bed.Her early
morning stiffness was severe in such a way that she used to take the
help of his husband while getting up from the bed .
After few
days she developed pain in the left proximal interphalangeal joints,
which gradually progressed to wrist joint , elbow , ankle and meta
tarsophalangeal joint.
No history of hair loss, oral ulcerations ,rash over the face.
No history of thickening of the skin.
No history of cough and shortness of breath.
Past history:
No significant past history.
Family History:
No significant family history.
General examination:
Examination:
Pulse Rate: 80 beats per minute
Blood Pressure: 100/60 mmhg
Respiratory Rate: 22 cycles per minute
Temperature: 98.6 F
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema
General Examination:
Hair:
Normal hair distribution.
Eyes:
No erythema noted on conjunctiva .
Oral Cavity:
No mucosal ulcers
Nails:
No nail pitting, onycholysis, onychodystrophy
Skin:
No
rash , ulcers over the skin, scaly lesions, dryness of skin, thickening
of skin, no rash on sun exposed areas of the skin, no subcutaneous
nodules.
Spine:
No spinal deformity
Musculoskeletal examination: ( positive findings)
Tenderness noted in the MCP joints of both fingers
Right Little finger: Boutonniere deformity
Left little finger: Swan neck deformity.
Boutonniere deformity of little finger
Investigations:
X ray both hands including wrist joints:
X ray both feet :
Chest x ray :
Bilateral reticulonodular opacities noted in both lungs
Respiratory System: No abnormality detected
Cardiovascular System: No abnormality detected
Abdomen: No abnormalities detected
Nervous System: No abnormalities detected
Investigations:
CUE -
ALBUMIN - NIL
SUGAR - NIL
PUS CELLS -NIL
EPITHELIAL CELLS - NIL
CBP -
HB - 12.0
TLC - 9,000
MCV - 82.1
PLATELETS - 3.02 LAKHS
NCNC
RBS - 106
LFT -
TB - 0.60
DB - 0.19
AST - 15
ALT - 212
ALP - 136
TP - 6.4
RFT -
UREA - 14
CREATININE - 0.8
URIC ACID - 3.8
Ca+ - 9.4
Phosphate - 2.6
Na + - 143
K+ - 3.7
Cl - 105
Other investigations :
C reactive protein - 2.4mg/dl.( Reference range -0.6mg/dl)
RA factor - Positive (96IU/ML) .
ESR - 33mm/1st hour.
Provisional Diagnosis:
Multiple
symmetrical polyarthritis with chronic duration of around 7 years and
with signs of inflammation, involving PIP joints and MCP joints with
sparing of DIP joints - Rheumatoid Arthitis
with no other system involvement.
Treatment:
1) Tab Methotrexate 10 mg/ PO/weekly once .
2) Tab Folic acid 5mg / PO/weekly once.
3) Tab HCQ( Hydroxy chloroquine 200mg)/PO/ Once daily.
4) Tab Naproxen 250mg /PO/SOS.
----------------------------------------------------------------------------------------------------------------
SHORT CASE II
Chief compliants:
Absent Menstrual cycle 6 months back.
History of present illness :
Patient
was apparently asymptomatic 6 months back, then she developed absent
Menstrual cycles not associated with any pain abdomen and vomtings and
then she went to the gynecology OPD and on routine evaluation , the
ultrasound abdomen showed altered renal echotexture and Urine analysis
showed Proteinuria and she was referred to general medicine department
for further work up.
No history of any rash over the malar areas, ulcers in the mouth and pain in the joints.
No history of any hematuria , throat pain, skin rashes.
No history of fever ,pain abdomen , cold etc.
No history of any pedal edema , shortness of breath and decreased urine output
No history of any loss of appetite, dryness of skin and vomtings .
Past history:
No history of similar complaints in the past.
History of seizures at around 2 years of age.
GENERAL EXAMINATION:
No pallor ,icterus,clubbing,cyanosis,lymphadenopathy.
Pedal edema.
SYSTEMIC EXAMINATION:
BP: 100/80
PR: 70BPM
CVS:S1S2+
RS; BAE+
P/A: SOFT,NON TENDER
Clinical images :
Investigations:
LFT -
TB -0.7
DB - 0.12
AST - 10
ALT - 08
ALP - 238
TP - 6.2
ALB - 4.19
RFT
UREA - 43
CREATININE - 3.7
URIC ACID - 7.8
Ca + - 9.6
Phosphate - 3.7
Na - 145
K+ - 4.1
Cl- 103
CUE -
ALBUMIN - 3+
RBC - 1-2
Crystals - 2+
CASTS - NIL
PUS CELLS - NIL
CBP -
HB - 9.8
TLC - 8,600
PCV - 29.4
RBC - 3.51 MILLION
PLTS - 1.66 LAKHS
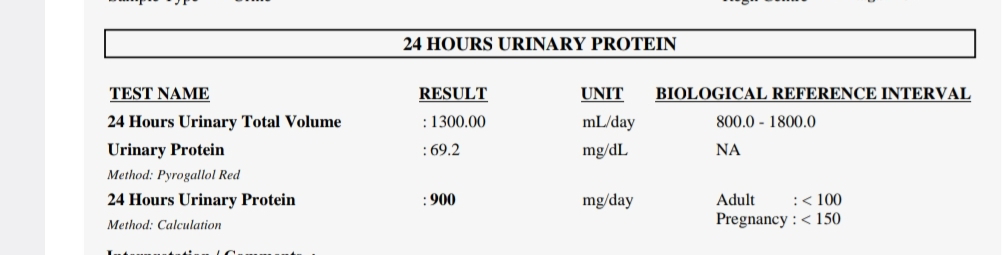
24 hour urinary protein was 900mg/ day.
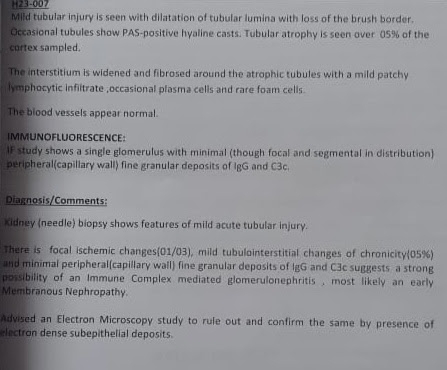
Renal biopsy:
Electron microscopy:
Treatment:
1) Tab Mycophenolate mofetil 360mg /PO/TID.
2) Tab Minipress XL /PO/OD
3) Tab Bisoprolol 2.5mg /PO/OD .
Critical appraisal:
https://pubmed.ncbi.nlm.nih.gov/36745456/
P -The role of mycophenolate mofetil (MMF) in management of immunoglobulin A nephropathy (IgAN)
I-total
of 170 participants were randomized in a 1:1 ratio to receive MMF
(initially, 1.5 g/d for 12 months, maintained at 0.75-1.0 g for at least
6 months) plus SC or SC alone.
C- During a 3-month run-in period, 238 patients received optimized supportive care (SC), including losartan
O-This
study found that addition of MMF to SC compared with SC alone
significantly reduced risk of disease progression among patients with
progressive IgAN.
























Comments
Post a Comment