20100006007 CASE PRESENTATION
LONG CASE
CHIEF COMPLAINTS:-
- THE PATIENT MET WITH AN ACCIDENT ON 7.03.23 (HOLI)
- WEAKNESS IN BILATERAL UPPER AND LOWER LIMBS SINCE 3 MONTHS
- RETENTION OF URINE SINCE 3 MONTHS
-DECREASED SENSATION ON LOWER LIMBS - 3 MONTHS .
History of present illness:-
The patient was apparently asymptomatic 3 months back then he met an RTA skid and fall from 2 wheeler on 7.03.23 (Holi) around 9:00pm. As soon as the accident happened, he got unconscious and was taken to a local hospital, where it was said that he injured his back. According to the patient, he was unconscious for a whole day. After regaining conciousness, the patient was unable to move both of his legs, was able to partially flex his elbow to a certain extent. The patient was unable to clench his fists completely on both sides, with the left hand having more power than the right. There was pain on both of the wrists, radiating to all of the fingers and being throbbing in type, and continuous in nature. However currently, the progression of the intensity of the pain is decreasing and the patient is able to clench his fists on both sides to some extent.
The patient also mentions experiencing hip pain due to the injury he has sustained when he was in the hospital. This pain lasted for two to three days, and disappeared after that.
On 10.03.23, the patient was admitted to another hospital where the following investigations were done:-
1) NCCT of the brain was done. it has ruled out the presence of any head injury.
2) MRI OF SPINE spine was done, which suggested disc bulges (lesions) at L4-L5, L5-S1 and C3-C4, C4-C5.
The Patient was later advised to undergo physiotherapy.
Upon admission to the OPD, the patient presented with the following symptoms:-
1) the patient was unable to use both the lower limbs voluntarily. The severity of the condition is a paresis and the progression of the condition is static and chronic. He was not able to sit initially after the accident but now he can sit on his own without an attendant.
2) Slight neck pain felt when patient is lifting his head. Pain is described as throbbing type, and aggrevated when the patient is lifting his head.
3) he also complained of tightness around the abdomen (Band like sensation/girdle like sensation)
4) The patient also complained of retention of urine able to feel the fullness of the bladder but is unable to initiate micturition for which a catheter is inserted since 2 months.
Other observations include:-
1) The patient was unable to comb the hair since the time of the accident, but he able to take the food to the mouth by himself.
2) The patient was unable to button the shirt by himself since the time of the accident.
3) The patient was able to squat and getting up from the squatting position with help, but he cannot climbing stairs up and down or walk by himself.
4) The patient cannot perform slipping of chappals, and there is no tripping of toe.
5) The patient with help, can roll over the bed, and get up from the bed.
6)No Difficulty in breathing.
7) There is no diurnal variation of weakness.
Negative history
No h/o visual disturbances, headache, diplopia, ptosis he is able to appreciate smell, hes able to look towards all sides no h/o sensory loss over the face, no facial deviation.
No noted sensory deficit as the patient was able to feel clothes, feeling hot and cold water while bathing.
No h/o auditory disturbances
No h/o restricted tongue movements
No difficulty in swallowing
No difficulty in speaking
No h/o abnormal sweating
No h/o shooting pain
No h/o headache or vomiting.
No h/o seizures
No h/o Fasciculations/muscle twitchings.
No h/o Involuntary movements like chorea, athetosis, tremors, hemiballismus
TREATMENT HISTORY:
No specific treatment
PERSONAL HISTORY :
MARITAL STATUS: Married
DIET: Mixed
APPETITE: NORMAL
SLEEP: irregular and inadequate
Bowel movements: irregular
Bladder: Unable to pass urine since 3 months
No history of any allergens
Addictions :
Alcohol consumption since 8 yrs (2 quarters daily )
Tobacco chewing since 6 yrs
FAMILY HISTORY :
Not significant
GENERAL EXAMINATION
Pt is conscious, coherent, cooperative moderately built, and moderately nourished
No H/O of
Pallor
Icterus
cyanosis
clubbing
Lymphadenopathy
Edema
VITALS :
Temp: Afebrile
PR: 86 bpm
Rr:18 cycles /min
BP: 130/80 mm of hg
SYSTEMIC EXAMINATION :
RESPIRATORY SYSTEM :
Trachea Central
NVBS
No murmurs
CVS
S1 and s2 sounds heard
No cardiac murmurs
ABDOMINAL EXAMINATION :
shape - scaphoid
Tenderness- no
Palpable mass - no
Liver - not palpable
Spleen - not palpable
Bowel sounds - normal
NEUROLOGICAL EXAMINATION :
Higher mental function
The patient is conscious well oriented to time place and person
No delusions or hallucinations
Dominant right hand
Cranial nerve examination:
CN 1 : smell sense RIGHT LEFT
+. +
CN 2 : visual acuity normal Normal
CN 3 4 6 : extra ocular movement : full
Direct light reflex present
Consensual light reflex present
Ptosis absent
Accommodation reflex present
CN 5 : Sensory : over face ,buccal mucosa : normal
Motor: masseter ,temporalis : normal
Reflexes :corneal : normal
Conjunctival : normal
CN7 : Motor : nasolabial fold : present
Reflexes: corneal conjunctival present
CN 8: Rinnes +
Webers not lateralised
Nystagmus : absent
CN 9 and 10 : uulva movemts normal
Motor system:
BULK: Inspection : Decreased
Palpation : Decreased
CNS EXAMINATION:-
Bulk
rt lf
Arm 23 cm 23cm
Forearm 24cm 24cm
Leg 29cm 29cm
Tone
rt lf
Arm increased increased
Leg increased increased
Power
rt lf
Deltoid 5 5
Supraspinatus 5 5
Infraspinatus 5 5
Pectoralis major +4 +4
Biceps 5 5
Brachioradialis 5 5
Triceps -4 -4
ECR 5 5
ECU 5 5
Extensor digitorum -4 -4
FCU 3 -4
Abductor pollicis longus -4 +4
EPB -4 +4
Opponens pollicis -unable to do on both-
Abductor pollicis brevis 3 +4
Adductor policis -4 4
Lumbricals and interossei
Test one -4 -4
Test two 3 3
Lower limbs
Illeopsoas 3 -4
Adductor femoris -4 +4
Gluteus medius and minimus 5 5
Gluteus maximus 3 3
Hamstrings +4 -4
Quadriceps +4 +4
TA -4 +4
TP +4 +4
Peronius -4 +4
Gastrocnemius +4 +4
EHL +4 -4
Extensor digitorum longus 3 3
Flexor Digitorum Longus 5 +4
Reflexes :
SUPERFICIAL:
Plantar not visualized
Abdominal reflexes -mute
DEEP TENDON REFLEXES :
Rt Lft
Biceps : + 3 +3
Triceps: +3 +3
Supinator: +3 +3
Knee jerk: +3 +3
Ankle jerk: +2 +2
SENSORY SYSTEM :
Posterior column:
fine touch - normal
Vibration - normal
SPINO THALAMIC :
Pain : decreased sensation to pain in lower limbs
Temperature: decreased sensation to heat and cold in lower limbs
CEREBELLAR SIGNS :
Finger nose test : normal
Heel knee test : unable to touch
MENINGEAL SIGNS
neck stiffnesses. Absent
Kernigs sign - absent
Brudzinski sign - not visualised
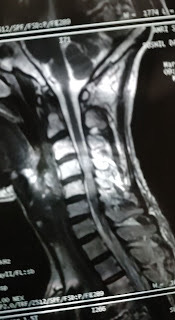
MRI OF SPINE :
Diffuse disc bulges are seen at L4-L5, and L5-S1 levels, causing secondary spinal stenosis.
Diffuse disc bulges are seen at C3-C4, and C4-C5 levels, causing secondary spinal canal stenosis with mild narrowing of bilateral neural foramina with mild impingement of bilateral exiting nerve roots.
PROVISIONAL DIAGNOSIS :
CHRONIC POST TRAUMATIC ASSYMETRICAL ( RIGHT MORE THAN LEFT ) SPASTIC QUADRIPARESIS WITH UMN BLADDER.
----------------------------------------------------------------------------------------------------------------
A 26 year old female graduated in MSc chemistry presented to our outpatient unit with the complaints of
Multiple joint pains since the past 2 years.
Present Illness:
A 26 year old female was apparently asymptomatic 2 years back after which she started experiencing multiple joint pains. She reported that she first experienced right proximal interphalangeal joint pain 2 years back. After 2 weeks she started to experience left proximal interphalangeal joint pain. Over the last 2 years, she started experiencing multiple joint pains - bilateral meta-carpophalangeal joints, with involvement of bilateral elbow joint, bilateral ankle joints ( intermittently). She reported early morning stiffness lasting for more than an hour which would be relieved on physical activity. She would experience these pains intermittently and would often be accompanied by swelling of the joint and would be relieved on taking pain medications. She reported that she developed bilateral little finger and Ring finger ( 4th and 5th PIP) deformity 1 and half year back.
She however gave no history of fever, oral ulcers, rash, dryness of the skin, hair loss, any development of rash on exposure to sunlight, discouloration of skin on exposure to cold.
No other constitutional symptoms like fever, fatigue, weight loss.
Past History:
No other significant past history
Personal History:
She is happily married and gravida with 10 weeks of Gestation. She has a good appetite, normal bowel and bladder movements.
Family History:
No significant family history
Provisional Diagnosis:
Chronic, multiple, symmetrical joint involvement, involvement of PIP & DIP joints - ? Rheumatoid Arthritis
Examination:
Pulse Rate: 75 beats per minute
Blood Pressure: 120/70mmhg
Respiratory Rate: 22 cycles per minute
Temperature: 98.6 F
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema
General Examination:
Hair:
Normal hair distribution, normal texture, colour
Eyes:
No conjunctival injection, no erythema, no corneal lesions
Oral Cavity:
No mucosal ulcers
Nails:
No nail pitting, onycholysis, onychodystrophy
Skin:
No rash , ulcers over the skin, scaly lesions, dryness of skin, thickening of skin, no rash on sun exposed areas of the skin, no subcutaneous nodules
Spine:
No spinal deformity
Musculoskeletal System Examination:
Gait: Normal
Musculoskeletal system:
Upper limbs:
Boutenniere' or button hole deformity of the right ring finger & little finger ( 4th & 5th PIP)
This is the case of an 82-year-old female who presented to the hospital with chief complaints of
- Fever since 5 days
- Pain in the left knee joint since 2 days,
- Swelling in the left knee joint since 2 days
History of presenting illness:
The patient was apparently asymptomatic 6 months ago.
6 months ago, the patient experienced a pricking type of joint pain while climbing the stairs, it was pricking in nature, and the patient could carry out her daily activities without hindrance.
On 25th May 2023, After waking up at 5 AM, the patient could not lift her legs from the bed. The patient explains that she had to drag her feet to the washroom.
In a matter of three days, the patient developed a sudden onset of pain. The pain was pricking in character, and continuous. present bilaterally in the lower limbs at and below the level of the knee. It aggravated on walking and relieved at rest.
The pain was associated with swelling of the lower limb at and below the level of the knee joint, bilaterally. It was associated with redness over the limbs.
The patient also experienced high-grade fever, which was continuous, and . not associated with chills and rigour. She also experienced generalised body pain and malaise.
2 Days later, the patient visited a doctor and was prescribed medications. The symptoms reduced after the consumption of medicines.
One week later, there was a sudden increase in pain and swelling similar to the last episode. There was also a rise in fever up to 104 degrees Fahrenheit.
The patient came to our hospital and was given, NSAIDS, paracetamol,normal saline and antibiotics. This resulted in a reduction of symptoms, and the patient was discharged.
2 Days later, the patient developed the same constitution of symptoms again and came to our hospital.
Past History and treatment history
The patient is a known case of hypertension since 10 years and has been on Telmisartan and Amlodipine since then.
10 years ago, the patient had a history of trauma, that led to a fracture of the ulna.
8 Months ago, the patient had a syncopal attack and was started on low-dose aspirin as a prophylactic measure.
The patient is not a known case of Diabetes Mellitus, Tuberculosis, CAD, or Epilepsy.
The patient consumed NSAIDs when she experienced pain.
She was prescribed Diethyl Carbamazine, on her first visit to the doctor since 15 days.
She was prescribed amoxicillin seven days ago.
Family History
Brother and sister have asthma.
Personal History
Appetite: reduced since yesterday
Diet: Vegetarian
Sleep: The patient consumes alprazolam (on prescription) as she has difficulty falling asleep.
Bladder: 9 months ago, the patient had oliguria, since the onset of fever, she has increased the frequency and urgency of micturition.
Bowel Movements: Normal
Addictions: None
Allergies: none.
General Examination
The patient is conscious, coherent, and oriented to time, place and person.
The patient is moderately built and moderately nourished.
Vitals :
- Pulse - 94 beats per minute
- RR- 16 cycles per minute
- Temperature: Afebrile
-Blood Pressure- 120/70 mmHg
Pallor - Present



















Comments
Post a Comment