20100006008 CASE PRESENTATION
LONG CASE
70 year old male who is a resident of Nalgonda who is survived with two kids caste to the casualty with complaints of :
1. Weakness of right upper limb and lower limb since 6 months
2. Slurring of speech since 6 months
2006: Patient was apparently asymptomatic 25 years back then he observed right lower limb weakness for which he was given home remedies and was subsided by 2 months was able to go to work by 2months
2013 : Patient had met with an RTA and sustained fracture to his left femur and was operated in Hyderabad underwent internal fixation .
After 6 months from this incident , he couldn’t go to work due to his fracture , his sons and wife would go for farming , and he would be at home taking rest , he started walking using walker , one night he went to a function in the near by village ate non -veg and drank alcohol 90ml and came back home and complained left sided chest pain to his sons and wife at 3:00pm and near by practice right was called for check up where he told his bop shoot up to 200/100mmhg , he advised for immediate hospital admission , due to lack of transport they got him to the hospital after 6 hours , by then he developed right hemiparesis and complainted of slurring of speech with deviation of mouth .
No History of Numbness, tingling. *Nausea, vomiting, diarhhoea, *Involuntary movements, * wasting/thinning , *Band like sensation , * low back ache , *cotton wool sensation *postural giddiness, palpitation, * seizure, *Head trauma , *loss of perception of smell, *Blurring of vision/ double vision * loss of sensation over face , *Difficulty in chewing food, * Abnormality in taste sensation.
PERSONAL HISTORY:
He wakes up at 5 am in the morning goes to the farm and work there till 8am and come back to home and freshen up for 1 hour eat and go back to work and comes back by 4 pm
His appetite was normal and takes mixed diet, sleep adequate, bowel and bladder movements were regular.
General examination:
Patient is conscious, non-coherent, co-operative ,oriented to person , moderately built and poorly nourished.
Pallor - Negative , Icterus- negative, No cyanosis ,clubbing ,Lymphademopathy, pedal edema.
VITALS:
Bp: 140/90 mmhg
Pr :80bpm regular normal volume in right supine position
spo2 :98%at room air
Temp :97°F
RR -18cpm
Grbs -136gm/dl
Cvs -s1 s2 heard,no murmurs
Rs -bae +,nvbs heard
P/a soft ,non-tender,
bowels sound heard
CNS:
HMF- patient conscious, orientation is not elicited
Speech- motor aphasia(+) .
No h/o delusions, hallucinations.
h/o emotion lability.
cranial nerves: Right left
1 st: smell Could be elicited
2nd :VA/colour-Vision: Couldn’t be elicited
3rd,4th,6th:
pupil size. N N
DLR/CLR. Couldn’t be elicited
No ptosis, nystagmus : Couldn’t be elicited
5th :
sensory: over face and buccal mucosa : Couldn’t be elicited
motor : mastication movements : Couldn’t be elicited
reflex : corneal and conjunctival (+)
Jaw jerk (-).
7th:
motor:
Nasolabial Lost on the right side Present on left side
Fold prominent.
Facial mov. Weakened Normal
sensory: Couldn’t be elicited
Secretomotor: moistness of eye +
Tongue : normal, buccal mucosa normal.
8 the nerve:
Rinnes : Couldn’t be elicited
Weber's: Couldn’t be elicited
9and 10 th nerve:
uvula centrally placed and symmetrical, gag and palatal reflex present
11 th nerve:
trapezieus : Couldn’t be elicited
sternocleidomastoid : Couldn’t be elicited
12th nerve:
tongue tone normal, no wasting, no fibrillations,no deviation of tongue.
MOTOR SYSTEM :
Right. Left
Bulk: Upper limb Normal Normal
Lower limb Normal Normal
Tone: Upper limb: Hypotonia Normal
Lower limb : Hypotonia Normal
Power: Upper limb : 0/5 5/5
Lower limb : 2/5 5/5
Reflexes:
Superficial reflexes:
Right. Left
Corneal- (+) (+)
Conjunctival- (+) (+)
Abdominal- (-) (-)
Plantar- Decreased Decreased
Muscle power :
Upper limb : Couldn’t be elicited
Lower limb : Couldn’t be elicited
Deep tendon reflexes :
Right. Left
Biceps. ++++ ++
Triceps. ++++ ++
Supinator. ++++ ++
Knee ++++ ++
Ankle. ++++ -
SENSORY SYSTEM:
Not elicited due to motor aphasia.
CEREBELLUM:
titubation - absent
Nystagmus- absent
Intensional tremors - absent
Hypotonia-no
Pendular knee jerk : Couldn’t be elicited
Dysdiadokinesia : Couldn’t be elicited
MENINGIAL SIGNS:
Neck stiffness - negative
Kernigns sign - negative
Brudzinkis sign - negative
PROVISIONAL DIAGNOSIS
Acute ichaemic stroke with denovo RVD+
INVESTIGATIONS
HAEMOGRAM
Hb-13.3 gm/dl
TLC- 9,200
58/30/04/06/00
PCV- #39.8
MCV-88.2
MCH-29.4
MCHC-33.3
RBC COUNT-4.52 million/cu mm
PLATLETS COUNT- 3.24 lakhs/cu mm
BLOOD GROUP- B +ve
BT- 2 MIN 30 SEC
CT - 4 MIN 30 SEC
RFT
Urea-19
Creat-0.9
Uric acid-5.0
Ca-1.02
Phosphorus -3.2
Na- 138
K- 3.5
Cl-10.6
LFT
Total bilirubin -#1.13 mg/dl
Direct-#0.58mg/dl
AST- #56
ALT-#79
Alkaline phosphatase -#1053
Albumin-3.41
RBS -#87 mg/dl
FINAL DIAGNOSIS
Acute ischemic stroke in parietal, temporal and frontal regions with RVD+.
--------------------------------------------------------------------------------------------------------------------------------------
SHORT CASE I
20 year old female who is a student came to casuality with c/o -
* Pain abdomen since 2 days
* Vomitings since 2 days
* Hypopigmentated lesions over face since 4 months
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 2 days back, then she developed pain abdomen in epigastric region, radiating to back, relieved on bending forward, associated with vomitings - non bilious, non projectile ( 4 episodes) subsided on taking medicine.
History of similar complaints in the past, diagnosed with acute pancreatitis, 5 months ago and treated accordingly. No documents available
PAST HISTORY
H/O RTA 3 years back ( fracture to left femur)
where she was diagnosed to have Type 1 DM for which she was on insulin ( subcutaneous, Inj.Mixtard 12 U - X- 10 U) for a year.
Patient observed non compliance to insulin and was shifted to OHA by local hospital.(? Unknown drug)
Patient used OHA for 2 months and stopped in between and started on insulin in her own.
Due to pain abdomen, patient dropped taking insulin for a day
PERSONAL HISTORY
Diet- Mixed
Appetite - Normal
Bowel and Bladder- Regular
Sleep - Decreased due to pain
Addictions - None
General examination:
The patient is conscious, coherent and cooperative, moderately built and nourished, and is well oriented to time, place and person.
BMI- 25.6 Kg/m2
Pallor: absent
Icterus: absent
Cyanosis: absent
Clubbing: absent
Koilonychia: absent
Pedal edema: absent
Lymphadenopathy: absent
JVP- No rise
Acanthosis nigrans- present over neck
Vitals:
Temperature: afebrile
Respiratory rate: 19cpm
Blood pressure: 120/80 mm Hg
Pulse: 102 bpm
RBS- 480 mg/dl
Systemic examination:
Cardiovascular system:
S1, S2 heard
No murmurs
Respiratory system:
BAE +
Trachea: central
Vesicular breath sounds heard
Central nervous system:
Patient is conscious
No focal neurological deficits
P/A
Soft, tenderness+ in epigastric region, no guarding/ rigidity, bowel sounds heard
PROVISIONAL DIAGNOSIS
Acute pancreatitis with type 1 diabetes
INVESTIGATIONS :
ECG
Chest X Ray
|
RFT |
HEMOGRAM |
CUE |
|
SERUM CREATININE: 0.7MG/DL |
HEMOGRAM: 13.0GM/DL |
COLOUR:PALE YELLOW |
|
BLOOD UREA:29MG/DL |
TLC:11,300CELLS/CUMM |
APPERANCE:CLEAR |
|
SERUM SODIUM:137mEq/L |
PLT:3.36LAKHS/CUMM |
|
|
SERUM POTASSIUM:4.5mEq/L |
|
PUS CELLS:3-4/HPF |
|
SERUM CHLORIDE :108mEq/L |
|
EPITHELIAL CELLS: 2-3/HPF |
|
|
|
ALBUMIN: NIL |
|
|
|
|
|
|
|
LFT: |
FLP |
|
|
SERUM LIPASE: 135 |
TB:1.52 |
TOTAL CHOLESTEROL:261MG/DL |
|
|
HbA1C: 6.9% |
DB:0.6 |
TRIGLYCERIDES :932MG/DL |
|
|
RANDOM BLOOD SUGAR: 382MG/DL |
AST/ALT:17/9 |
HDL:81MG/DL |
|
|
SERUM AMYLASE: 261 |
ALP:181 |
LDL:150MG/DL |
|
|
|
ALB:3.32 |
|
USG ABDOMEN
*Grade l Fatty liver
*Altered echotexture of pancreas with peripancreatic fat stranding likely acute pancreatitis
*Raised echogenicity
CECT ABDOMEN on 13-4-2023
*Pancreas is slightly bulky with peripancreatic fat stranding and peripancreatic fluid collection in inferior aspect of body of pancreas measuring 5.3 X 3.3 Cm associated with mild thickening of renal fascia bilaterally
*CT Severity index 6/10
Final diagnosis : Acute pancreatitis secondary to hypertriglyceridemia with type 1 DM
---------------------------------------------------------------------------------------------------------------------------------------
SHORT CASE II
60 year old female , ex farmer presented to casuality with c/o
* Pedal edema since 2 months
*Decreased urine output since 2 months
HISTORY OF PRESENTING ILLNESS
Patient is ex farmer by occupation , was apparently asymptomatic 2 months ago .
Patient was apparently asymptomatic 5 years back, then she met with RTA, Where she fell on the divider and sustained injury on right side of head.
CT showed bleed and was operated as per patient.? Craniotomy
-Intially she noticed b/l swelling of lower limbs , gradual onset and progressive . Pitting type and extending upto knees .
Not associated with shortness of breath
Associated with decreased urine output
Not associated with orthopnea and PND
No h/o chest pain , palpitations
In view of pedal edema , patient visited local hospital and was told ,She had a stone in one of her kidneys and both her kidneys failed .
She used NSAIDS for over 3 months I/v/o low backache.
She was advised maintenance hemodialysis,but patient denied and was discharged on medications .
Later, pedal edema subsided after using medications .
She continued taking medications , but noticed loss of appetite, fatigue and generalized weakness .
No h/o pus in urine , burning micturition , frothy urine .
As she had generalized fatigue ,loss of appetite and elevated urea and s. creatinine ,she visited our hospital and was initiated on hemodialysis by placing central venous catheter in right internal jugular vein .
Patient had 4 sessions of hemodialysis .
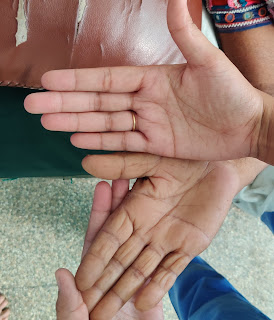
She went to Hyderabad and got A-V fistula on his left hand .
C/o Low back ache and body pains .
C/O abdominal distension since 5 days , sudden onset and progressed gradually . Associated with increased sob on lying down and abdominal tightness.
Pedal edema is mild extending upto ankle joint.
No h/o yellowish discoloration of eyes . No h/o binge alcohol intake .
PAST HISTORY
K/c/o HTN since 10 years and is not on regular medication .
NOT a k/c/o DM, TB , ASTHMA,CAD , EPILEPSY,CVA .
No surgical history and past Medical history
PERSONAL HISTORY
Regular bowel and bladder movements
Adequate sleep
Loss of appetite present
Mixed diet
FAMILY HISTORY - Not significant
Addictions - Toddy drinker occasionally -3 times /week . 90 ml
Non -Smoker
GENERAL EXAMINATION:
Pt C/C/C
No pallor, icterus , clubbing, cyanosis,koilonychia , lymphadenopathy
B/L pedal edema - pitting type present. extending upto ankle .
Jvp - couldn't be assessed due to central line .
Skin - Dry ,scaly , itching present .
Eyes - Grade 2 HTN retinopathy changes noted on fundoscopy .
Vitals :
Bp - 140/90 mmhg - Right arm supine posture
Pulse - 130 bpm ,regular ,normal volume, condition of vessel wall - normal, no radio-radial or radio-femoral delay.
Resp rate - 26/ min
Spo2 - 97% o
Grbs - 110 mg/dl
Temp -99 F
SYSTEMIC EXAMINATION :
GIT EXAMINATION :
INSPECTION :
Shape of abdomen - Distended-uniform
Flanks – Full
Umbilicus – Everted
Skin – Stretched, shiny
No scars, sinuses, striae, nodules , discoloration.
Dilated veins – absent
Movements of the abdominal wall - All quadrants equally moving with respiration .
Abdomino - Thoracic type of breathing
NO visible intestinal peristalsis
Hernial Orifices normal
Cough impulse - Negative
PALPATION
No local rise of temperature
No tenderness
Hernial Orifices - normal
Murphy’s Punch/Renal angle tenderness - no tenderness
PERCUSSION:
Fluid Thrill - Absent
Shifting dullness - Absent
AUSCULTATION:
Bowel sounds – Present
Aortic, Renal Bruit - Absent
CARDIOVASCULAR EXAMINATION :
INSPECTION:
Chest wall shape - Ellipsoid and b/l symmetrical
No Precordial bulge, Pectus carinatum/excavatum
No Kyphoscoliosis
No Dilated veins, scars, sinuses
Apical impulse - Visible in left 5 ICS 1 cm lateral to MCL .
Pulsations – epigastric, parasternal - absent
PALPATION:
Apical impulse – Tapping type , felt in left 5 ICS 1 cm lateral to
No Thrills and palpable heart sounds .
Auscultation :
S1 S2 heard in Aortic , pulmonary,tricuspid and mitral areas .
No added sounds
No murmurs
Respiratory system -B/L NVBS
CNS - NO abnormality detected
PROVISIONAL DIAGNOSIS
Chronic kidney disease secondary to NSAID abuse
INVESTIGATIONS
FINAL DIAGNOSIS
Chronic Kidney Disease with egfr 25 mL/ min square.