20100006009 CASE PRESENTATION
LONG CASE
30/F,homemaker,unmarried, hailing from chityal, who completed her bsc botany came with
COMPLAINTS :-
Lethargy-----> since 6 months
HISTORY OF PRESENT ILLNESS :-
Patient was apparently asymptomatic 6 months back then she had insidious onset of lethargy,
easy fatiguability on doing daily chores like cooking, cleaning the house.
No history of any fever, cough,Loss of appetitie,weight loss,chest pain, palpitations,pedal edema
No menstural abnormalities
PAST HISTORY :-
At her 17years of age(in year 2010),One afternoon while bathing, she suddenly developed weakness
of right upper limb and lower limb, along with deviation of mouth to left side upon which she made
sounds , her mother who was nearby came to her aid ,and she was taken to hospital in nalgonda
within an hour,and referred to gandhi hospital where she was admitted for 1month,during which her
speech returned.She was able to walk without support after 1month,but still has limp on walking.
Weakness of the right upper limb persisted,like unable to lift the hand,hold objects, stretch out.
This episode was not associated with blurring of vision, vomiting,headache,loss of consciousness tingling ,numbness, involuntary movements, swallowing difficulty.
4 years back in 2019 she presented to Kamineni narketpally with complaints of painful swelling
in the left side of the neck, for which usg guided fnac was done showing caseating
granuloma,started on ATT and used for 6 months.
No h/o hypertension,diabetes,thyroid disorders,coronary artery disease.
FAMILY HISTORY:-
No similar complaints in the family.she has one elder and one younger sister
PERSONAL HISTORY:-
Appetite is normal, diet consists of lentils,rice, vegetables, less of meat,eggs ,fruits.
GENERAL EXAMINATION :-
Patient is conscious, coherent,co-operative.Moderately built and nourished
Pallor +
Icterus -
Cyanosis -
Clubbing -
Lymphadenopathy + :posterior cervical ,lymph node ,mobile,non tender
-Contracture present at the right metacarpophalangeal joint.
VITALS :
Pulse:-90/min,right arm,regular rhythm,normal volume
Arteries Right. Left
Carotid. + +
Subclavian. +. absent
Brachial. +. absent
Radial. +. absent
Femoral. +. +
Popliteal. +. +
Posterior tibialis. +. +
Dorsalis pedis. +. +
Radio femoral delay. not present
Bruit: heard over right and left carotid artery
Blood pressure Right Left
upper limb 120/60mmhg. not recordable
lowerlimb. 100 mmhg systolic. 100 mmhg
Respiratory rate-22cycles per min
JVP-Not elevated
Grbs-120mg/dl
SYSTEMIC EXAMINATION
CENTRAL NERVOUS SYSTEM
Right/left handed person :initially right,then learnt to write with left hand since 12 years
Education:Bsc botany
HIGHER MENTAL FUNCTIONS :conscious,oriented
Memory: intact (immediate,recent,remote)
Speech:
comprehension:+
fluency+
repetition+
reading+
writing+
naming objects+
CRANIAL NERVES. Right. Left
1-olfactory: present. present
2-visual acuity: normal. normal
Visual field:confrontation method:normal
Colour vision:normal
Fundus: normal. normal.
3,4,6
eyelids :. normal. normal
position of eyeball at rest: normal. normal
extraocular movements :. normal. normal
pupil :size,shape normal. normal
direct and indirect light reflex: present. present
5:
sensory: touch. present. present
pain. present. present
temperature. present. present
motor: side to side jaw movement normal
reflexes: corneal. present. present
jaw jerk. present. present
7th-
motor- frontalis. normal. normal
orbicularis oculus: normal. normal
orbicularis oris: deviated to the left
buccinator:. decreased. normal
sensory: taste:. normal. normal
8th: Rinnie's. normal. normal
Weber's :No lateralization
9th,10th-
Position of uvula:central
Gag reflex present. present.
11th- SCM-. normal. normal
Trapezius-. normal. normal
12th-
Tongue: size,symmetry,
normal. normal
MOTOR SYSTEM:
Attitude of limbs:
Upper limb.
Right Left
Semi- Flexion at elbow Normal
Semi pronated
Thumb tucked into palm
Lower limb.
Semi -flexed at knee. normal
Bulk:arm:
forearm:. 24cm. 25cm
Thigh:. 38cms. 39cms.
Tone:
upperlimb. increased normal
lowerlimb. increased. normal
Power:
1)Neck:. flexors:. normal. normal
extension:. normal. normal
2) shoulder: Supraspinatus. 4-/5. 5/5
Deltoid:. 4-/5. 5/5
Infraspinatus:. 4-/5. 5/5
Latissimus dorsi :4-/5. 5/5
Serratus anterior: 4-/5. 5/5
Pectoralis major:. 4-/5. 5/5
Rhomboids 4-/5. 5/5
3)elbow: biceps. 4-/5. 5/5
Triceps. 4-/5. 5/5
Brachioradialis. Not able to pronate 5/5
4) wrist : flexor carpi radialis Not able to flex 5/5
flexor carpi ulnaris. Not able to flex 5/5
extensor carpi radialis longus: Not able to extend 5/5
extensor carpi ulnaris longus. Not able to extend 5/5
extensor digitorium : Not able to extend 5/5
Handgrip. 60%. 100%
Abductor pollicis longus. Not able to abduct 5/5
Abductor pollicis brevis. Not able to abduct 5/5
Extensor pollicis longus. Not able to extend 5/5
Extensor pollicis brevis. Not able to extend 5/5
Opponens pollicis. Not able to perform. 5/5
Adductor pollicis. Not able to adduct 5/5
Lumbricals Not able to Perform 5/5
Interossei -dorsal. Not able to Perform 5/5
palmar. Not able to Perform 5/5
5)Trunk:abdominal
Beevor's - absent
6)Hip: Iliopsoas. 4+/5. 5/5
Adductor femoris. 4+/5. 5/5
Gluteus medius 4+/5. 5/5
Gluteus Maximums. 4+/5. 5/5
7)knee: flexion: hamstrings. 4+/5. 5/5
extension: quadriceps 4+/5. 5/5
7) Ankle: Plantar flexion:. Not able to perform 5/5
Dorsiflexion:. Not able to perform 5/5
Reflexes:
Superficial
corneal. present. present
abdominal. present. present
plantar:. extensor. flexion
Deep
biceps. 3+. 2+
supinator. 3+. 2+
triceps. 3+. 2+
knee jerk. 3+. 2+
ankle jerk. +1. +1
No clonus
Sensory:. in all dermatomes
fine touch. present. present
joint position. present. present
vibration. present. present
crude touch. present. present
pain. present. present
temperature. present. present
Romberg's test: negative(no sway)
cerebellum:
finger nose. Not able to perform normal
finger finger. Not able to perform normal
knee heal. normal. normal
rebound phenomenon- absent
tandem walking. - normal
Gait :-Gait Video
circumduction on the right,
Toes touching the ground first
pace:normal
falling to sides:absent
hand swing:. absent present
turn:. normal
Autonomic nervous system:normal
Meningeal signs:absent
CARDIOVASCULAR SYSTEM :
-Elliptical & bilaterally symmetrical chest
-No visible pulsations/engorged veins on the chest
-Apex beat seen in 5th intercostal space medial to mid clavicular line
-S1 S2 heard
-No murmurs
RESPIRATORY SYSTEM
Upper respiratory tract normal
Lower respiratory tract :
-Left supraclavicular fullness present
-Trachea is central
-Movements are equal on both sides
-On percussion resonant on all areas
-Bilateral air entry equal
-Normal vesicular breath sounds heard
-No added sounds
-Vocal resonance equal on both sides in all areas
PER ABDOMEN :
-Scaphoid
-No visible pulsations/engorged veins/sinuses
-Soft,non tender, no guarding and rigidity, no organomegaly
-Bowel sounds heard,No abdominal Bruit
2010
Hb: 7.5gm/dl,TLC-8500 cells/mm3, adequate platelets
Ana:negative
2d echo:normal
Serum creatinine:0.9mg%
CHEIF COMPLAINTS
55yr male Tiles construction worker came with complaint of
Generalised weakness :- 2 months
Fever :- 2 months
Dry cough :-2 months
HISTORY OF PRESENT ILLNESS
Patient was apparently alright till 2months back then he had insidious onset of fever, intermittent, relived on taking medications,not associated with chills and rigors.
Fever is associated with generalised weakness(not able to perform his previous routine job works) and dry cough(which is insidious onset, intermittent,relived on taking medication, no aggravating factors, not associated with positional or seasonal variation)
History of weight loss, loss of appetite present.
No history of coughing of blood, chest pain, palpitations,swelling of lower limbs, facial puffiness, decreased urine output
PAST HISTORY
History of pulmonary tuberculosis 25years back,used ATT for 6months.No history of interventional procedures done during that period.
Not a known case of DM/HTN/CAD/CVA/EPILEPSY/Thyroid disorder/Retroviral illness
PERSONAL HISTORY
Takes alcohol 90ml whisky per day for past 30years
Tobacco chewer for 30years
Takes mixed diet,appetite decreased from past 2months,regular bowel and bladder movements,adequate sleep
FAMILY HISTORY
No history of similar illness in the family
GENERAL EXAMINATION
Patient is conscious, coherent,co-operative
Moderately built and nourished
No Pallor,Icterus,Cyanosis,Clubbing,Lymphadenopathy,Pedal edema
Oral candidiasis +
Spine deformity-Dorsal thoracic vertebra Gibbs +
VITALS :-
PR:-80bpm,regular rhythm,normal volume, all peripheral pulses felt
BP-110/80mmhg,In right upper limb sitting position
RR-28/min,Abdominothoracic type, regular
Temperature:99 F
SPO2 : 99% on Room air
Grbs-120mg/dl
JVP-Not elevated
SYSTEMIC EXAMINATION
RESPIRATORY SYSTEM
Upper respiratory tract :
Nose--external nose normal, no deviated nasal septum
Oral cavity--Poor oral hygiene,Oral thrush +
Lower respiratory tract :
Inspection :
-Trachea appears to be in centre
-No scars, sinuses,dilated veins over the chest
-Apical impulse not visible
-Chest-Bilaterally symmetrical/Elliptical
-Chest movement Decreased on right side
-On examining back of the chest in standing position, with arms hanging by the side of the body
No drooping of shoulder
Spinal deformity present -->Dorsal thorassic vertebrae Gibbus +
Palpation :
-Trachea--Central
-Apex beat--1.5cm medial to mid clavicular line in the left 5th intercostal space
-Respiratory movements --decreased on right side with respiration
-Chest Measurements :
Anteroposterior diameter-18cm
Transverse diameter-28cm
Ratio of AP diameter : Transverse diameter :
Chest circumference :85cm
Vocal fremitus : Increased on right side of chest
Percussion : Resonant
Auscultation:
Supraclavicular & Infraclavicular : Bronchial breath sounds +
Vocal Resonance:increased on right side of chest
Added sounds :
Inspiratory crepts present on the right side of chest
OTHER SYSTEM EXAMINATION
CARDIOVASCULAR:
-Elliptical & bilaterally symmetrical chest
-No visible pulsations/engorged veins on the chest
-Apex beat seen in 5th intercostal space medial to mid clavicular line
-S1 S2 heard
-No murmurs
PER ABDOMEN :
-Scaphoid
-No visible pulsations/engorged veins/sinuses
-Soft,non tender, no guarding and rigidity, no organomegaly
-Bowel sounds heard
-Cranial nerves - intact
-Sensory system-normal
-Motor system -normal
PROVISIONAL DIAGNOSIS :
?Re-activation of pulmonary Tuberculosis
INVESTIGATIONS
Radiological
CBP
Hb-10.4gm/dl
TLC -5400cells/cumm
Plt - 1.98lakhs/cumm
LFT
TB-1.2 mg/dl
DB-0.3 mg/dl
AST-88 IU/L
ALT-72 IU/L
ALP-553 IU/L
TP-8.3gm/dl
ALB-2.9gm/dl
RFT
Sr Na/k/cl--133/4.3/96
Sr cr-1.2mg/dl
Sr urea-41mg/dl
RBS-94mg/dl
Serology
--------------------------------------------------------------------------------------------------------------------------------------CHEIF COMPLAINTS
40yr female farmer by occupation came with complaint of
Pain in the both hips (Since 6 months)
Pain in the both hands Finger joints on & off (Since 6months)
HISTORY OF PRESENT ILLNES
Patient was apparently alright 6months back,then she developed pain in the both hip regions which is insidious onset,gradually progressive,aggrevated on walking,getting up from sitting posture,Pain relived on taking medications.
Associated with Pains in the multiple small joints of both hands on and off.No history of early morning stiffness,heel pain.
PAST HISTORY
Patient had history of multiple hospital admissions due to hypokalemic paralysis over past 3years
1st episode :-In 2020,Pt developed weakness of right lower limb, taken to hospital found out to be potassium low, after correction, she recovered
Asymptomatic between
2nd episode :-In NOV 2021,Paraperesis,Potassium was low,Recovered after correction
3rd episode : In May 2022,Quadriparesis,Potassium was low,Intubated and connected to ventilator in view of respiratory paralysis.Discharged after 7days
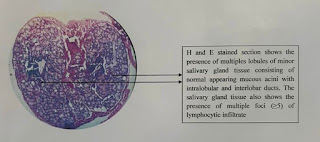
4 Months back patient had burning sensation of both eyes which is aggravated on watching TV,cellphone and excessive thirst(bcz of drying of tongue) associated with left parotid gland swelling.With these symptoms patient came to the hospital, eye examination revealed severe dry eye.In view of connective tissue disorder(?sjogren syndrome), Lower lip biopsy was done.Histopathology report shows lymphocytic infiltration of minor salivary glands
DRUG HISTORY
Patient is started on prednisolone tablets 4months back.She used regularly for 1month then after only during severe pains
FAMILY HISTORY
No similar complaints in the family members
PERSONAL HISTORY
Takes mixed diet,appetite normal,regular bowel and bladder movements,adequate sleep.No addictions
GENERAL EXAMINATION
Patient is conscious, coherent,co-operative.Moderately built and Moderately nourished.
Blood pressure-130/70mmhg,right arm, supine position
Pulse-90/min,regular rythm,normal volume, all peripheral pulses felt
Respiratory rate-20/min
Temperature-98 F
Spo2-98% on room air
Grbs-125mg/dl
No pallor,icterus,clubbing,cyanosis,lymphedenopathy,edema of legs
No raised JVP
HEAD TO TOE EXAMINATION
-Elliptical & bilaterally symmetrical chest
-No visible pulsations/engorged veins on the chest
-Apex beat seen in 5th intercostal space medial to mid clavicular line
-S1 S2 heard
-No murmurs
PER ABDOMEN :
-Scaphoid
-No visible pulsations/engorged veins/sinuses
-Soft,non tender, no guarding and rigidity, no organomegaly
-Bowel sounds heard
-Cranial nerves - intact
-Sensory system-normal
-Motor system -normal
-Gait --- Waddling Giat +
Chest x ray
X ray pelvis
RBS - 101mg/dl
CUE
PH - 7.0
Color - pale yellow
Appearance - clear
Reaction - acidic
Specific gravity -1.01
Albumin - trace
Sugars - nil
Bile salts - nil
Bile pigments - nil
Pus cells : 3-4
Epithelial cells : 2- 3
RBC - nil
Crystals - nil
Casts - nil
RFT
Urea - 16mg/dl
Creatinine - 1.3mg/dl
Uric acid - 3.1 mg/dl
Calcium - 10.1mg/dl
Phosphorus - 2.6mg/dl
Sodium - 141mEq/L
Potassium - 3.6 mEq/L
Chloride - 105 mEq/L
LFT
Total bilirubin - 0.67mg/dl
Direct bilirubin - 0.12mg/dl
SGOT - 14 IU/L
SGPT -11 IU/L
Alkaline phosphatase - 492 IU/L
Total proteins - 6.6 gm/dl
Albumin- 4.02gm/dl
A/G ratio 1.56
ESR - 30mm/ 1st hour
ABG




































































Comments
Post a Comment